Neurological Rehabilitation for Parkinson's Disease and the Vestibular System
We offer you a thorough assessment, modern technology and individually tailored rehabilitation to improve function and slow down negative development.


Do the motor or non-motor complaints hinder your everyday life?

In Parkinson's disease, vestibular dysfunction is an often underestimated contributor that both causes and worsens motor and non-motor symptoms.
When the brain processes and coordinates balance signals from the inner ear poorly with vision, gaze control, and movement in the neck and back. This impairs gaze stability, visual orientation, concentration, coordination, postural control, and responsiveness. The result can be worsening rigid movements and tremors, poor balance and responsiveness that increase the risk of falls and freezing of movements, and dizziness.
At Brain Camp, we objectively map this with advanced computer equipment and tailor targeted rehabilitation. The goal is to improve function and slow the negative development of symptoms.


"Kim Tore Johansen treated me for Parkinson's which involves a number of ailments and challenges. Kim Johansen made a thorough and analytical assessment of my medical challenges and created an individual plan for me to effectively and quickly reduce my
Parkinson's challenges. I have been to treatment on 2 different weeks with about 3 months between and my challenges have been significantly reduced”
Treatment course
We offer comprehensive and thorough assessments to map the brain's functional challenges caused by Parkinson's disease, including computer-based tests that objectively measure the function of the vestibular system.
A comprehensive and thorough assessment is carried out to map and understand your condition and what treatment you need.
After 2-3 treatment sessions, re-testing is performed using data-driven tests to evaluate progress.
When re-testing shows improvement, you will receive thorough training on how to do the exercises yourself for a period of time. This includes written and video instructions on how to perform the exercises correctly.
We will follow you closely during the period of exercises at home before you return for a new re-test to assess whether you are ready for the next phase of rehabilitation.
What makes us unique?
How we help you
A comprehensive and thorough assessment using advanced computer-based equipment is required to identify which parts of the brain and nervous system have the greatest functional challenges. This provides an understanding of which parts of the brain and nervous system must be prioritized first to achieve the best possible effect from tailored neurological rehabilitation.
Parkinson's disease affects not only the parts of the brain involved in controlling body movements, but also parts of the brain that are essential for the ability to have good orientation, coordinate and process different sensory inputs, control over gaze, and concentration.
QEEG
QEEG is an advanced method for analyzing the electrical activity of the brain during rest. It involves comparing the recorded brain wave patterns with a normative database to identify abnormalities in brain activity. QEEG provides a more nuanced understanding of brain function by assessing factors such as brain wave amplitude, frequency, coherence, and connectivity between different brain regions.
Computerized Measurement of Eye-Hand Coordination
Computer-based measurement of eye-hand coordination is a test that measures how the brain integrates visual perception with motor and cognitive responsiveness and precision. This test provides good information about the brain's ability for cognitive processes such as spatial understanding, reaction time and decision-making.
Databases Balance measurement
Computerized balance measurement measures how well the brain processes and coordinates different movement information from all sensory organs, and how well the brain is able to multitask several balance and motor challenges simultaneously. Including movement information from the muscles and joints in the feet, hips, pelvis and back, neck and balance organ in the inner ear, and visual movement.
vHIT
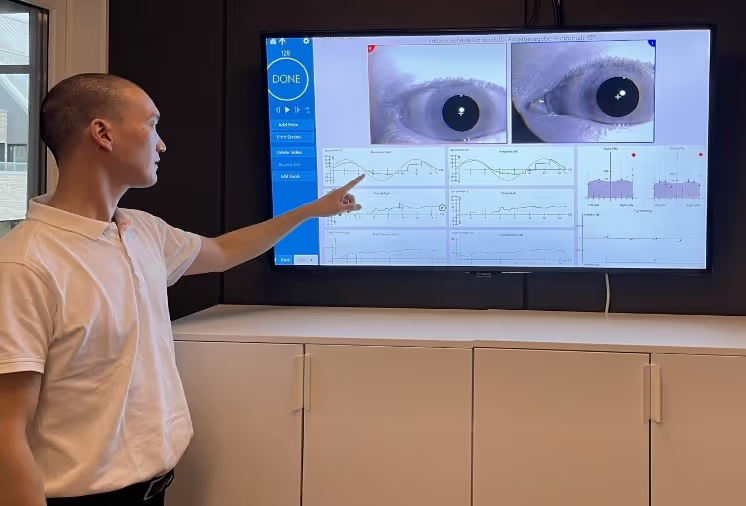
Video head impulse test is a computer-based test that measures the brain's ability to process movement information from the balance organ in the inner ear together with movement information from the neck, and align and coordinate gaze with head movements. This test provides important information about the brain's ability to process and align vestibular information with movement information and visual information in the present tense. Which is essential for being able to move smoothly and balanced without falling or stopping movements, and to provide correct perception of movement.
Saccadometry
Saccadometry measures rapid purposeful eye movements and gives us more detailed information than VNG about parts of the brain that are involved in, among other things, responsiveness, and coordination and precision of purposeful movements.
Videonystagmography (VNG)
Using VNG, we measure fine motor control and coordination over purposeful movements with the gaze. This includes tests that challenge steady gaze fixation, calm following movements that we use when we follow people or objects moving in our environment, and rapid movements that we use when we scan our environment to plan movements or when we read. This advanced computer-based test gives us objective information about the function of parts of the brain that are involved in, among other things, motor skills, coordination, processing and integration of different sensory inputs, responsiveness, and concentration.
Our therapists
Brain Camp has extensive experience in examining and adapting rehabilitation for children and adults with disorders resulting from neurological disease and acquired brain injury. We base our approach on the latest neuroscience research and use advanced computer-based equipment to detect functional disorders of the brain and nervous system.

Frequently Asked Questions About Treatment of Parkinson's Disease and the Vestibular System
-4970 NOK/430 EUR
Treatment/neurological rehabilitation:
-From 1425 NOK/123 EUR
Re-test/Re-evaluation:
-From 2925 NOK/253 EUR
Treatment of BPPV in the TRV Chair:
-1930 NOK/167 EUR
5 day rehabilitation stay
-From 40,000 NOK/3,455 EUR (travel and accommodation are additional)
Monday morning we start with a thorough examination to map out the functional disorders of the nervous system and brain, followed by a thorough review of what your examination shows. Including a review of findings from the computer-based tests that show how the brain and nervous system function.
If you are accompanied by a close relative, we always recommend that the relative joins us when we review the findings. Relatives find this very useful in gaining a better understanding of your health situation. If you are not accompanied by a close relative, but your close relative is still interested in having your findings reviewed, the relative can join you via video call. You will then have a 1 ½ hour break before we start your first treatment, which lasts 30-40 minutes.
Your treatment will continue on Tuesday morning followed by the first re-test which includes, among other things, the various computer-based tests to confirm whether the brain and nervous system are responding as expected. In many cases, it is seen that the brain and nervous system are incorrectly compensating, and several tests become worse. Then we have to change and fine-tune the treatment program and then re-test again after 2-3 treatments on the same day or the next day. These re-tests are the key to being able to tailor your neurological rehabilitation. This process continues throughout the week until we have identified the most effective treatment program that affects your brain and nervous system in the best possible way, and gives you the best possible potential to improve symptoms and quality of life.
On Friday, we dedicate 3 sessions to teaching you how to perform the tailored home exercises on your own. If you need help performing the exercises, your travel companion will also receive thorough training on how to perform the exercises. This includes both written instructions and video instructions on how to perform the home exercises 3-5 days a week, with 1-2 sessions per day lasting anywhere from 5 minutes to 30 minutes.
Friday ends with a new re-test and re-evaluation to get a final evaluation of how the home exercises affect the brain and nervous system. We then have a good foundation to create a customized rehabilitation plan for the next 3-5 months before you should come back for a new rehabilitation stay. This is not the last day of treatment, but the start of a customized rehabilitation plan and close cooperation.
Includes close follow-up via email or phone during the first few weeks to ensure the best possible effect. There may then be a period of 8-10 months between the second and third rehabilitation stays. Learn more about rehabilitation stays
For those who have the opportunity, we recommend that your closest relatives join you when we review your findings. Relatives find this very helpful in gaining a better understanding of your health situation.
We then create a tailored rehabilitation plan for the first 3 treatments lasting 30-40 minutes per session, followed by a re-test/re-evaluation immediately after the third treatment.
Re-testing includes, among other things, the various computer-based tests to confirm whether your brain and nervous system are responding as expected. In many cases, it is seen that the brain and nervous system incorrectly compensate, and several tests become worse. Then we have to change and fine-tune the treatment and exercises and then re-test again after 2-3 treatments.
When re-tests show satisfactory changes, we create customized home exercises based on the treatment plan that best improves your tests.
The home exercises are performed 3-5 days a week, with 1-2 sessions per day lasting anywhere from 5 minutes to 30 minutes.
The patient works on the exercises themselves for 4-6 weeks before we re-test/re-evaluate to see if we can upgrade the rehabilitation plan.
However, the plan often needs to be further fine-tuned when you return home and start your home exercises in combination with your regular everyday activities. We will then closely monitor your progress by changing the amount and intensity of your home exercises, as well as adjusting your general activity level over the course of a day and week.
In most cases, following up via email is sufficient, but in some cases we need to arrange a telephone or video consultation to get enough information to further tailor the rehabilitation plan. Even if you go home and work on exercises on your own, you are not alone. We will follow you closely.