We treat concussions and whiplash injuries
We offer you a thorough examination, modern technology and individually tailored treatment for lasting recovery.


Are you struggling with delayed effects after a concussion or whiplash injury?

Concussions and whiplash injuries cause complex dysfunctions in your brain that make it challenging to process and coordinate multiple sensory inputs at once. This affects the brain's ability to activate the different areas with different functions at the same time that are necessary to interpret your surroundings and how you are moving, to distinguish between the environment or things around you that are moving and your own physical movement, to perform smooth and coordinated physical movements, and cognitive and executive functions. These dysfunctions in the brain cause further secondary malfunctions in your brain.
Where parts of the brain that are not normally activated during certain tasks become activated, while other parts of the brain that are normally activated remain passive or are activated too little. The combinations of these primary and secondary functional disorders may explain why over 40% of those who sustain a concussion develop persistent problems that prevent them from participating normally in work and leisure activities for more than 5 years.
Our approach is based on research showing that tailored neurological rehabilitation that addresses both primary and secondary functional impairments has significantly better efficacy in improving symptoms and tolerance to activity, even if you have been suffering from post-concussion syndrome for 3 years or more without having had any effect from previous treatment.



"I spent 2 years being evaluated by a number of doctors. No one knew what was wrong with me, but in the end I found the miracle Kim Tore Johansen. After my first day at the clinic, he knew what needed to be done. Here you feel seen, heard and understood. He and his team give me treatment with unique exercises that work. I received before and after tests between treatments. Then you could see clear progress. With regular home exercises, I had better stamina, less head fog, less headaches and the hallucinations disappeared."
How we help you
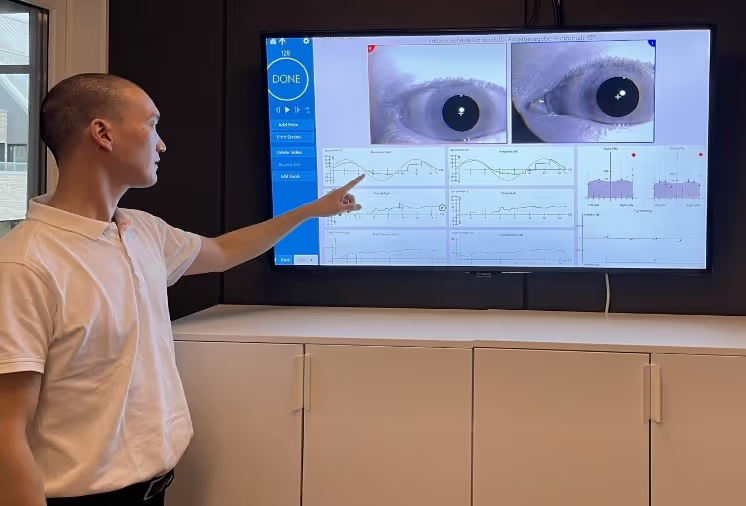
Our rehabilitation philosophy is that it is essential to have a broad and comprehensive functional examination with advanced computer-based equipment to map both primary and secondary functional disorders in your brain and nervous system in order to obtain the most information possible about how your rehabilitation should be initiated.
A comprehensive and thorough assessment is carried out to map and understand your condition and what treatment you need.
After 2-3 treatment sessions, re-testing is performed using data-driven tests to evaluate progress.
When re-testing shows improvement, you will receive thorough training on how to do the exercises yourself for a period of time. This includes written and video instructions on how to perform the exercises correctly.
We will follow you closely during the period of exercises at home before you return for a new re-test to assess whether you are ready for the next phase of rehabilitation.
What makes us unique?
Post-Commotio Syndrome has six subgroups
A comprehensive and thorough assessment is required to identify which subgroup you belong to. In most cases, there is an overlap of several subgroups, with one dominating. Identifying which subgroup you belong to is crucial for tailored rehabilitation.
Anxiety & Mood Post-Commotion Syndrome
In the case of a concussion and post-concussion syndrome, the limbic system – the brain's emotional and survival center – can be significantly affected. The concussion causes functional disorders in several of the areas responsible for limbic functions.
In the event of a concussion and post-commotio syndrome, the limbic system – the brain's emotional and survival center – can be significantly affected.
Concussion causes functional impairment in several areas responsible for limbic functions. Including areas called the amygdala, hippocampus, and prefrontal cortex , which are crucial for emotion regulation, stress response, memory and social behavior . This can lead to symptoms such as increased irritability, anxiety, depression, emotional instability, reduced motivation and stress intolerance . At the same time, the connections between the limbic system and the autonomic nervous system are affected, which can lead to disturbed sleep, inner unrest, hypersensitivity to sensory impressions and a reduced ability to regulate the body's physiological stress response . These functional disorders may explain why many with post-concussion syndrome experience that emotional, cognitive and physical complaints often reinforce each other and persist over time. Anxiety&Mood post-concussion syndrome is therefore characterized by increased anxiety, depression, mood swings and sleep problems.
Just as there is no specific area of the brain that is responsible for performing a specific cognitive or executive task, there is no specific area that is solely responsible for a limbic reaction. But a complex and harmonious cooperation between several parts of the brain at the same time. Including the cerebellum which has important functions in coordinating and regulating emotional reactions, stress response and emotional learning.
Cognitive Post-Commotio Syndrome
In cognitive post-concussion syndrome, there are clear challenges with specific cognitive and executive functions. Among other things, concentration, processing and working memory. There is not a specific area of the brain that is responsible for performing a specific cognitive or executive task, but a complex and harmonious cooperation between several parts of the brain at the same time.
In cognitive post-concussion syndrome, there are clear challenges with specific cognitive and executive functions. Among other things, concentration, processing and working memory. There is not a specific area in the brain that is responsible for performing a specific cognitive or executive task, but a complex and harmonious cooperation between several parts of the brain at the same time. Although there is no specific area that is solely responsible for a function, there are some specific areas in the brain that have more responsibility than others during certain actions. For example, fine motor movements are coordinated by the cerebellum, the cerebellum is also involved in coordinating the activity between the different parts of the brain that are involved in cognition and execution. The cerebellum ensures, among other things, the correct attention and pace in information processing, and contributes to accuracy and timing in mental processes.
It is not only a well-coordinated, smooth and harmonious activity between the different parts of the brain responsible for cognition and execution that is necessary to have good cognitive and executive abilities. The brain and nervous system must also be able to collect, filter, process and coordinate different forms of sensory input simultaneously in an effortless and efficient way in order to produce good and effective cognitive and executive actions. So an injury or dysfunction in, for example, the vestibular system, which involves the production of movement signals in the balance organ in the inner ear and the transmission of these movement signals to the parts of the brain responsible for collecting, filtering, and processing these movement signals. And also at the same time coordinating this movement information with other parts of the brain responsible for balance and orientation. Will not only trigger symptoms such as dizziness and impaired balance, but can also cause challenges with cognitive and executive tasks.
Post-Traumatic Migraine Post-Commotio Syndrome
The development of post-traumatic migraine is most likely due to a stress reaction resulting from the above-mentioned functional disorders, which leads to disturbed regulation of the autonomic nervous system. This disturbed regulation of the autonomic nervous system triggers a chain reaction of further functional disorders.
The development of post-traumatic migraine is most likely due to a stress reaction resulting from the above-mentioned functional disorders, which leads to disturbed regulation of the autonomic nervous system. This disturbed regulation of the autonomic nervous system triggers a chain reaction of further functional disorders.
- Prolonged contraction of blood vessels (vasoconstriction) after stress or strain.
- A reflexive widening of blood vessels (vasodilation).
- Overactivation of centers in the brainstem involved in sensitivity to the face, the trigeminal nerve, which releases the neuropeptide CGRP and creates inflammation around the brain's blood vessels in addition to facial pain.
- Reduced attenuation of the parasympathetic nervous system, which means that blood vessels and inflammation do not calm down, which prolongs the migraine attack.
- Disturbed baroreflex that regulates blood pressure when the body changes position, which causes blood pressure fluctuations, dizziness and headache sensitivity.
Because the uncontrolled contractions and dilations of blood vessels can affect any part of the brain and brainstem, there is also a wide range of symptoms that migraines can cause. The most common and well-known symptoms include:
- Headache.
- Dizziness.
- Stiffness and pain in the neck.
- Sound and light shadow.
- Nausea.
- Visual disturbances.
- Exhaustion.
But migraines can also affect other parts of the brain and brainstem, leading to more unfamiliar symptoms:
- Loss of vision in part or the entire field of vision.
- Language difficulties or loss of language.
- Stomach pain and diarrhea.
- Muscle spasms.
- Muscle paralysis
- Impaired balance.
- Faint.
Cervical Post-Commotion Syndrome
Neck problems after a concussion are very common, and as mentioned earlier, the mechanism of injury in a concussion is the same as in a whiplash injury. However, it is only in a third of whiplash cases that structural damage to the neck can be seen.
Neck pain after a concussion is very common, and as mentioned earlier, the mechanism of injury is the same for a concussion as for a whiplash injury. However, it is only in a third of cases of whiplash that structural damage to the neck can be seen. Several professional communities therefore suspect that chronic neck pain and the accompanying neck-related pain are due to complex dysfunctions in the parts of the brain and nervous system that are involved, among other things, in the control of stabilizing muscles and the large muscles of the back and neck. This includes parts of the brain and nervous system that are involved in filtering, recognizing, processing and coordinating movement information from joints and muscles in the neck and jaw joints, movement information from the balance organ in the inner ear, visual movement information, and movement information from joints and muscles from the body, arms and legs. To filter, recognize, process and coordinate different movement information properly and effortlessly. The brain must also have good abilities to activate and communicate with the different areas of the brain and nervous system that are involved in activating and controlling the core muscles of the neck and the muscles that control conscious movement of the neck to function normally. This includes, in addition to the areas of the brain that receive the different types of movement information, areas that are directly involved in, among other things:
- Send activation signals to the muscles in the neck and jaw joint.
- Coordinate muscle movements with the neck and jaw joints.
- Coordinate muscle movements in the neck with muscle movements of the eyes.
- Balance and the ability to walk and move the head and neck while standing still or in motion.
In concussion and post-concussion syndrome, one or more functional disorders in this complex circuit result in poor control of core muscles, increased static muscle tone in the neck and jaw joints, impaired ability to recognize neck movements, impaired control of the bite reflex, and impaired ability to coordinate and process movement information from other parts of the sensory system. The classic symptoms of these functional disorders are:
- Stiffness and pain in the neck and jaw joint.
- Weakness and poor tolerance to neck movement.
- Tension headache.
- Dizziness.
Oculomotor Post-Commotion Syndrome
Oculomotor post-concussion syndrome involves dysfunction in parts of the brain and nervous system that are involved in controlling and coordinating purposeful and reflexive eye movements.
Oculomotor post-concussion syndrome involves dysfunction in parts of the brain and nervous system that are involved in controlling and coordinating purposeful and reflexive eye movements. From centers in the brainstem that are involved in keeping the gaze fixed on an object, to centers in the brain that are involved in concentration, responsiveness, and coordination. Dysfunction in one or more areas that are involved in controlling and coordinating eye movements not only leads to visual disturbances in the form of blurred or double vision, and discomfort when reading and using screens. One can also experience impaired concentration, reading and learning difficulties, brain fog and dizziness, dizziness, and difficulty with tasks that involve the gaze.
Vestibular Post-Commotio Syndrome
Vestibular post-concussion syndrome involves functional disorders in the filtering, processing, and coordination of movement signals from the balance organ in the inner ear.
Vestibular post-concussion syndrome involves dysfunction in the filtering, processing, and integration of motion signals from the balance organ in the inner ear. This also involves integration of motion information from the muscles and joints in the neck along with fine motor control and coordination of reflexive eye movements. This involves the ability to filter and recognize head movement, which is important for distinguishing whether you are moving or standing still, and the ability to maintain gaze stability on an object while the head and neck are moving through the vestibulo-ocular reflex (VOR) and cervico-ocular reflex (COR), which are important for maintaining gaze stability when moving or reading. Good function of the VOR and COR is also essential for good visual and physical orientation when you are moving. Dysfunction of the vestibular system leads to:
- Dizziness.
- Unsteadiness and impaired balance.
- Challenges with focusing the gaze.
- Challenges with visual orientation during movement.
Our therapists
Leading in concussion, whiplash and neurological rehabilitation.

Frequently asked questions about treatment of Post-Concussion Syndrome and Whiplash
The first examination lasts approximately 5 hours:
-4970 NOK/430 EUR
Treatment/neurological rehabilitation:
-From 1425 NOK/123 EUR
Re-test/Re-evaluation:
-From 2925 NOK/253 EUR
Treatment of BPPV in the TRV Chair:
-1930 NOK/167 EUR
5 day rehabilitation stay
-From 40,000 NOK/3,455 EUR (travel and accommodation are additional)
Monday morning we start with a thorough examination to map out the functional disorders of the nervous system and brain, followed by a thorough review of what your examination shows. Including a review of findings from the computer-based tests that show how the brain and nervous system function.
If you are accompanied by a close relative, we always recommend that the relative joins us when we review the findings. Relatives find this very useful in gaining a better understanding of your health situation. If you are not accompanied by a close relative, but your close relative is still interested in having your findings reviewed, the relative can join you via video call. You will then have a 1 ½ hour break before we start your first treatment, which lasts 30-40 minutes.
Your treatment will continue on Tuesday morning followed by the first re-test which includes, among other things, the various computer-based tests to confirm whether the brain and nervous system are responding as expected. In many cases, it is seen that the brain and nervous system are incorrectly compensating, and several tests become worse. Then we have to change and fine-tune the treatment program and then re-test again after 2-3 treatments on the same day or the next day. These re-tests are the key to being able to tailor your neurological rehabilitation. This process continues throughout the week until we have identified the most effective treatment program that affects your brain and nervous system in the best possible way, and gives you the best possible potential to improve symptoms and quality of life.
On Friday, we dedicate 3 sessions to teaching you how to perform the tailored home exercises on your own. If you need help performing the exercises, your travel companion will also receive thorough training on how to perform the exercises. This includes both written instructions and video instructions on how to perform the home exercises 3-5 days a week, with 1-2 sessions per day lasting anywhere from 5 minutes to 30 minutes.
Friday ends with a new re-test and re-evaluation to get a final evaluation of how the home exercises affect the brain and nervous system. We then have a good foundation to create a customized rehabilitation plan for the next 3-5 months before you should come back for a new rehabilitation stay. This is not the last day of treatment, but the start of a customized rehabilitation plan and close cooperation.
Includes close follow-up via email or phone during the first few weeks to ensure the best possible effect. There may then be a period of 8-10 months between the second and third rehabilitation stays. Learn more about rehabilitation stays
For those who have the opportunity, we recommend that your closest relatives join you when we review your findings. Relatives find this very helpful in gaining a better understanding of your health situation.
We then create a tailored rehabilitation plan for the first 3 treatments lasting 30-40 minutes per session, followed by a re-test/re-evaluation immediately after the third treatment.
Re-testing includes, among other things, the various computer-based tests to confirm whether your brain and nervous system are responding as expected. In many cases, it is seen that the brain and nervous system incorrectly compensate, and several tests become worse. Then we have to change and fine-tune the treatment and exercises and then re-test again after 2-3 treatments.
When re-tests show satisfactory changes, we create customized home exercises based on the treatment plan that best improves your tests.
The home exercises are performed 3-5 days a week, with 1-2 sessions per day lasting anywhere from 5 minutes to 30 minutes.
The patient works on the exercises themselves for 4-6 weeks before we re-test/re-evaluate to see if we can upgrade the rehabilitation plan.
However, the plan often needs to be further fine-tuned when you return home and start your home exercises in combination with your regular everyday activities. We will then closely monitor your progress by changing the amount and intensity of your home exercises, as well as adjusting your general activity level over the course of a day and week.
In most cases, following up via email is sufficient, but in some cases we need to arrange a telephone or video consultation to get enough information to further tailor the rehabilitation plan. Even if you go home and work on exercises on your own, you are not alone. We will follow you closely.