Persistent Postural-Perceptual dizziness
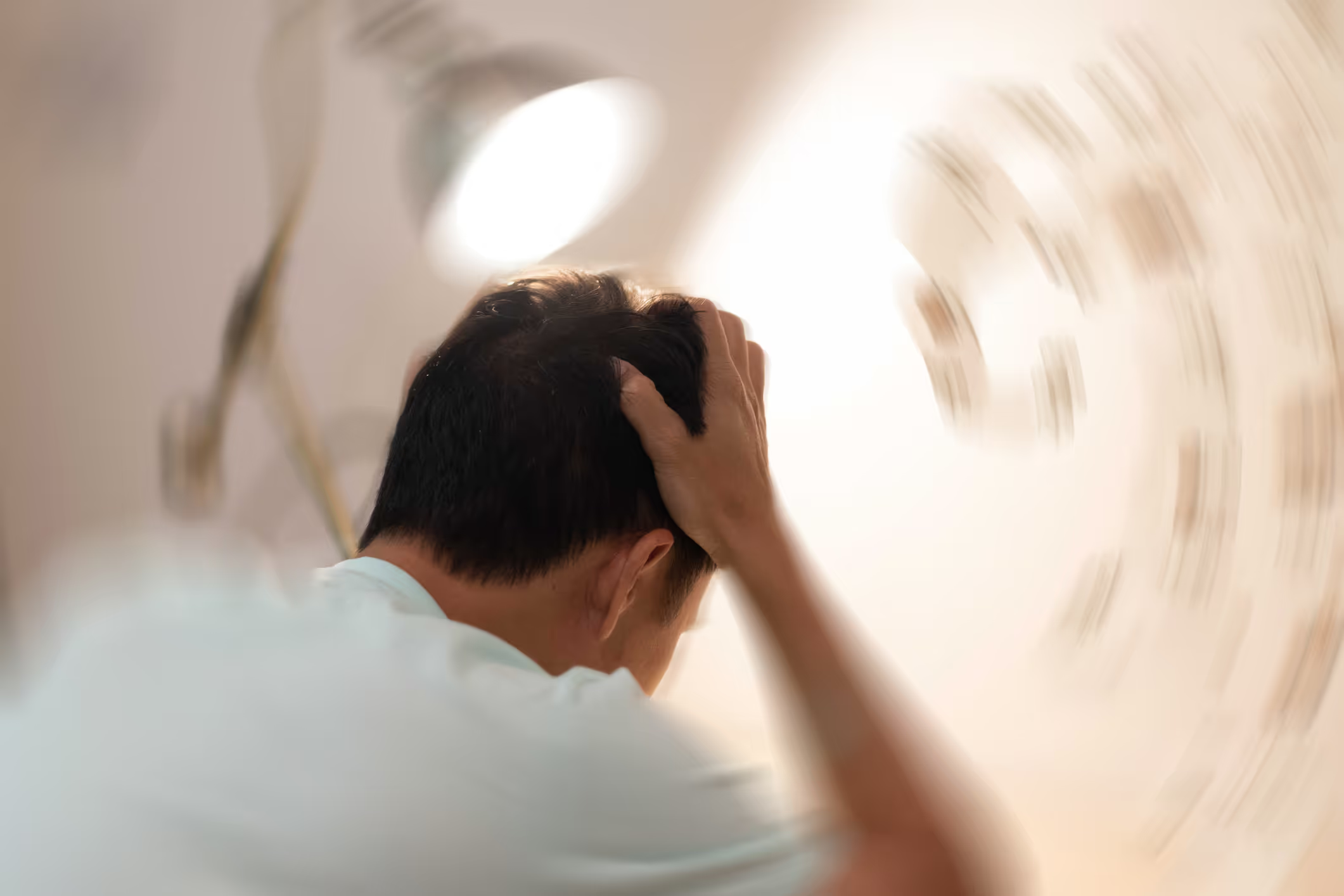
Persistent Postural Perceptual dizziness (PPPD) is a chronic functional vestibular disorder that causes a persistent feeling of unsteadiness and dizziness. Symptoms are often triggered by changes in body position or visual stimuli, and the condition can be severely disabling for quality of life and daily living. Although PPPD is not dangerous and there is no specific, direct structural damage to the vestibular system, the problem lies in the brain's ability to process and coordinate different sensory inputs. Recent research has given us better insight into the complex mechanisms behind PPPD, including sensory processing and integration disorders and their interaction with psychological factors.
What Causes PPPD?
PPPD usually develops after an acute vestibular event, such as vestibular neuritis (inflammation of the balance nerve), BPPV (dizziness), or vestibular migraine. Although the initial condition often resolves, the brain can become permanently dysfunctional, causing patients with PPPD to experience persistent symptoms that last for months or years. These include dizziness, unsteadiness and increased sensitivity to visual stimuli, fatigue, and decreased endurance for activity before symptoms are triggered or worsened.
The functional disorders behind PPPD
The brain dysfunction of PPPD is complex and involves multiple dysfunctional processes in the brain:
1. Sensory recalibration failing
Normally, after an acute vestibular event, the brain adapts by adjusting and recalibrating sensory systems to restore balance. In people with PPPD, this process fails, leading to an excessive reliance on visual cues to control movement and orientation. Even after the original disorder resolves, this maladaptive state persists, contributing to chronic symptoms.
2. Abnormal visual processing
People with PPPD have impaired perception of coherent visual motion. This makes it difficult for them to properly orient themselves and distinguish between physical movement and visual movement in environments with dynamic visual stimuli, which in turn can exacerbate feelings of unsteadiness and dizziness.
3. High sensitivity to Vestibular signals
Testing with galvanic vestibular stimulation (GVS) has found that people with PPPD have high sensitivity to vestibular signals. This increased sensitivity may explain why some patients experience increased dizziness even in situations with minimal vestibular stimulation.
4. Sensory mismatch and erroneous perceptions
Sensory mismatch is central to PPPD. This means that signals from the balance organ in the inner ear (vestibular system), visual systems, and movement signals from muscles and joints including the neck (somatosensory systems) are not coordinated or processed properly. The misalignment can lead to patients experiencing false perceptions of movement, which contributes to the worsening of symptoms.
5. Psychological factors
Anxiety plays a major role in PPPD. Increased anxiety levels caused by a lack of understanding of what is causing the dizziness can exacerbate the dizziness. This creates a self-reinforcing cycle. Anxiety and hypervigilance destabilize normal sensory integration, further exacerbating symptoms.
The functional disorders of PPPD consist of a complex combination of disturbed collection, processing and coordination of sensory information and psychological factors. On the one hand, disturbed coordination and processing of different sensory impressions, including visual and vestibular processing, creates a physiological basis for the disorder. The sensory system becomes more dependent on visual impressions for orientation, but the negative domino effect of functional disorders in the brain means that the brain also has challenges in distinguishing between visual movement and physical movement. The brain's calibration and compensation mechanisms fail, and any activity and sensory stimulation can trigger or worsen dizziness and other accompanying symptoms.
On the other hand, anxiety and avoidance behaviors contribute to intensifying and maintaining symptoms. Lack of understanding of what causes dizziness and what actually happens when dizziness is triggered or worsened can trigger anxiety that further intensifies the intensity of dizziness and accompanying symptoms. This combination of physiological and psychological factors makes PPPD a challenging disorder to treat.
Tailor-made Neurological Rehabilitation
To effectively treat PPPD, both the physiological and psychological components must be addressed. Brain Camp has extensive experience in tailoring neurological rehabilitation for people of all ages with PPPD. Our comprehensive examination, which includes several advanced computer-based tests, maps the brain's ability to collect, process and coordinate different sensory impressions so that we know which parts of the sensory system have the greatest challenges and may be the root of the dizziness.
The tailored neurological rehabilitation includes, among other things, individually adapted vestibular rehabilitation therapy and sensorimotor training, helping to improve and restore the brain's ability to coordinate and process different sensory impressions. To ensure that the brain and nervous system respond as desired, it is important to have frequent re-tests that reveal whether the brain is starting to work more correctly or whether the functional disorders are causing further miscompensations that, in the worst case, mean that rehabilitation has no effect or worsens dizziness. Our experience is that such miscompensations can be the reason why people with PPPD have not responded to previous rehabilitation. By finding a way to correct these miscompensations, we see that dizziness and accompanying symptoms gradually improve and quality of life returns.
Thorough explanation and education about the cause of dizziness is essential for managing dizziness and anxiety-provoking exacerbations. Including awareness of what triggers the anxiety-provoking exacerbation. In many cases, cognitive behavioral therapy (CBT) should also be included to help with this.

