Eye movements: A reflection of brain function

Neurological disease and brain disorders are more common than most people think. Statistics show that as many as 30% of the population are affected by diseases that affect the function of the brain at least once in their lifetime. This includes diseases such as stroke, Parkinson's disease, multiple sclerosis and traumatic brain injuries after car accidents or other forms of physical trauma.
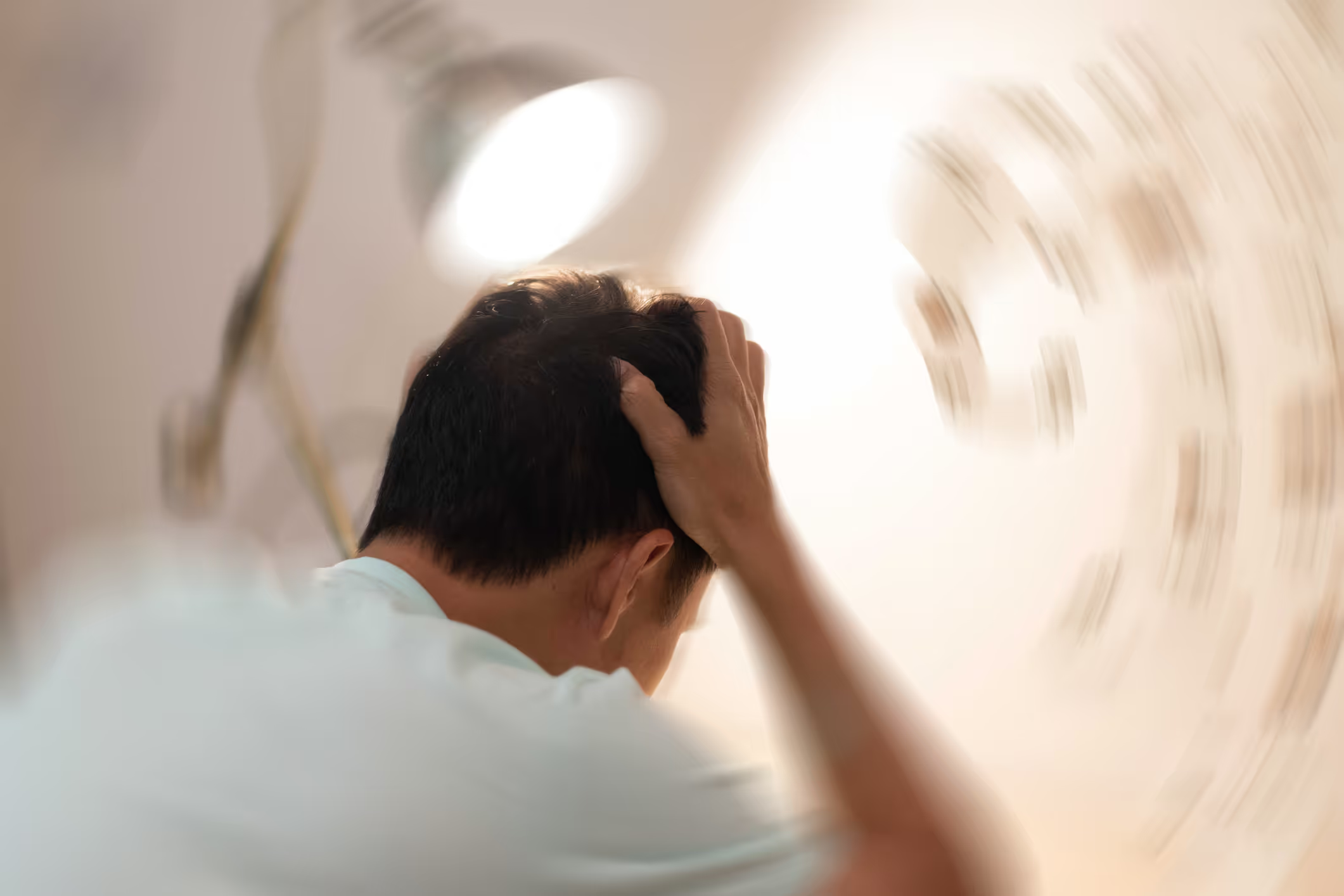
The various diseases and injuries to the brain can result in a number of different symptoms and functional impairments. Both visible physical disabilities such as muscle spasms and paralysis in an arm or foot, and invisible symptoms such as fatigue and dizziness. The physical disabilities are easier to understand and map than the "invisible" ones, as it is easy to measure muscle strength and mobility in the arms and legs. The invisible symptoms, on the other hand, can often be difficult to understand, map and measure if they are caused by functional disorders in the brain and nervous system. "Invisible" symptoms can include fatigue, brain fog, impaired concentration and memory, headaches, dizziness, hypersensitivity to sensory impressions and pain.
Fortunately, there have been great advances in brain research and how we can measure and train the function of the brain and nervous system after injury and disease. Since the late 19th century, much research has been conducted on the function of the brain and how eye movements can tell us the function of specific parts of the brain and nervous system. Research in this area, along with research into technology that can measure eye movements, has increased in recent years and given us a lot of important information about what happens in the brain during injury and disease. This includes a better understanding of the function of parts of the brain involved in physical movement, balance and coordination, processing of sensory impressions and cognitive and executive functions.
Among other things, researchers use videonystagmography (VNG) to measure various forms of eye movement. This examination equipment provides thorough data-based measurements of targeted fine motor eye movements by creating videos and graphs that make it easier and better to compare normal brain function with patients who have been exposed to brain injuries or diseases. Researchers also use these examination methods to assess whether treatment and rehabilitation have had the desired effect on brain function. Research conducted in several parts of the world shows that patients who have suffered a stroke have significantly reduced fine motor control over purposeful eye movements, along with reduced physical and cognitive function. At the same time, research also shows that improved fine motor control of purposeful eye movements after targeted neurological rehabilitation is associated with better recovery after a stroke. Both better physical and cognitive function.
The same type of studies have also been conducted on patients with brain injury after head trauma, multiple sclerosis (MS) and Parkinson's disease.
Thanks to this research, we now have several assessment tools that can provide us with objective test results that give us important information on how to tailor neurological rehabilitation, telling us whether rehabilitation has improved brain function and may have the potential to improve both motor and cognitive function.
Brain Camp uses video nystagmography (VNG) and other computer-based examination methods to tailor neurological rehabilitation. These tests also play an important role in assessing whether rehabilitation has had the desired effect on brain and nervous system function to provide the best possible potential in improving symptoms and quality of life.
We will write more about how different forms of targeted eye movements can tell us how the brain works, and how we use eye exercises to rehabilitate the brain and nervous system.
Reference list:
- Aasef G. Shaikh andDavid S. Zee, 2017. Eye movement research in the twenty-first century- a windowto the brain, Mind, and more. The Cerebellum. Published online December 19, 2017.
- Andrew T. Duchowski, 2002. A breadth-first survey of eye tracking application. Behaviorresearch methods, instruments & computers. November 2002, volume 34, issue4, pp 455-470.
- Delphine et al, 2016. The effect og short-lasting anti-saccade trainingin homonymous hemianopia with and without saccadic adaptation. Frontiers inbehavioural neuroscience, vol 9 (2016), article 332.
- Frederick R. Carrick et al, 2016. Eye-movement training result in changesin qEEG and NIH stroke scale in subjects suffering from acute middle cerebral artery ischemic stroke: A randomized control trial. Frontiers in neurology, vol7 (2016), article 3.
- Frederick R. Carrick et al, 2015. Evaluation of the effectiveness ofnovel brain and vestibular rehabilitation treatment modality in PSTD patientswho have suffered combat-related traumatic brain injuries. Frontiers in PublicHealth vol 3 (2015), article 15.
- Frederick R. Carrick et al, 2015. Short- and long-term effectiveness of asubject's specific novel brain and vestibular rehabilitation treatment modalityin combat veterans suffering PTSD. Frontiers in Public Health vol 3 (2015),article 151.
- Michael Gallaway etal, 2017. Vision therapy for post-concussion vision disorders. Optometry andvision science 2017, volume 94 (1), p 68-73.
- Juliana Bittencourtet al, 2013. Saccadic eye movement applications for psychiatric disorders.Neuropsychiatric Disease and Treatment 2013: 9 1393-1409.
- R. J. Leigh andChristopher Kennard, 2003. Using saccades as a research tool in the clinicalneuroscience. Brain (2004), 127, 460-477.
- Sally A. Jones andRoger A. Shinto, 2006. Improving outcome in stroke patients with visualproblems. Age and Ageing 2016; 35: 560-565.
- Tim Anderson, 2013. Could saccadic function be a useful marker of strokerecovery? Journal of neurology, neurosurgery and psychiatry. Published onlineJanuary 18, 2013.
- Timothy Belton and Robert A. McCrea (2000). Role of the CerebellarFlocculus Region in Cancellation of the VOR During Passive Whole body Rotation.Journal of Neurophysiology, 84: 1599-1613, 2000.
- Wei Dong et al,2012. Ischaemic stroke: the ocular motor system as a sensitive marker for motorand cognitive recovery. Journal ofneurology, neurosurgery and psychiatry 2013; 84: 337-341.
- Yasuo Terao et al,2017. What do eye movements tell us about patients with neurological disorders?An introduction to saccade recording in the clinical setting. Proceedingsof the Japan Academy. Series B, Physical and Biological Sciences2017; 93 (10): 772-801.