Chronic Positional Vertigo - Chronic BPPV
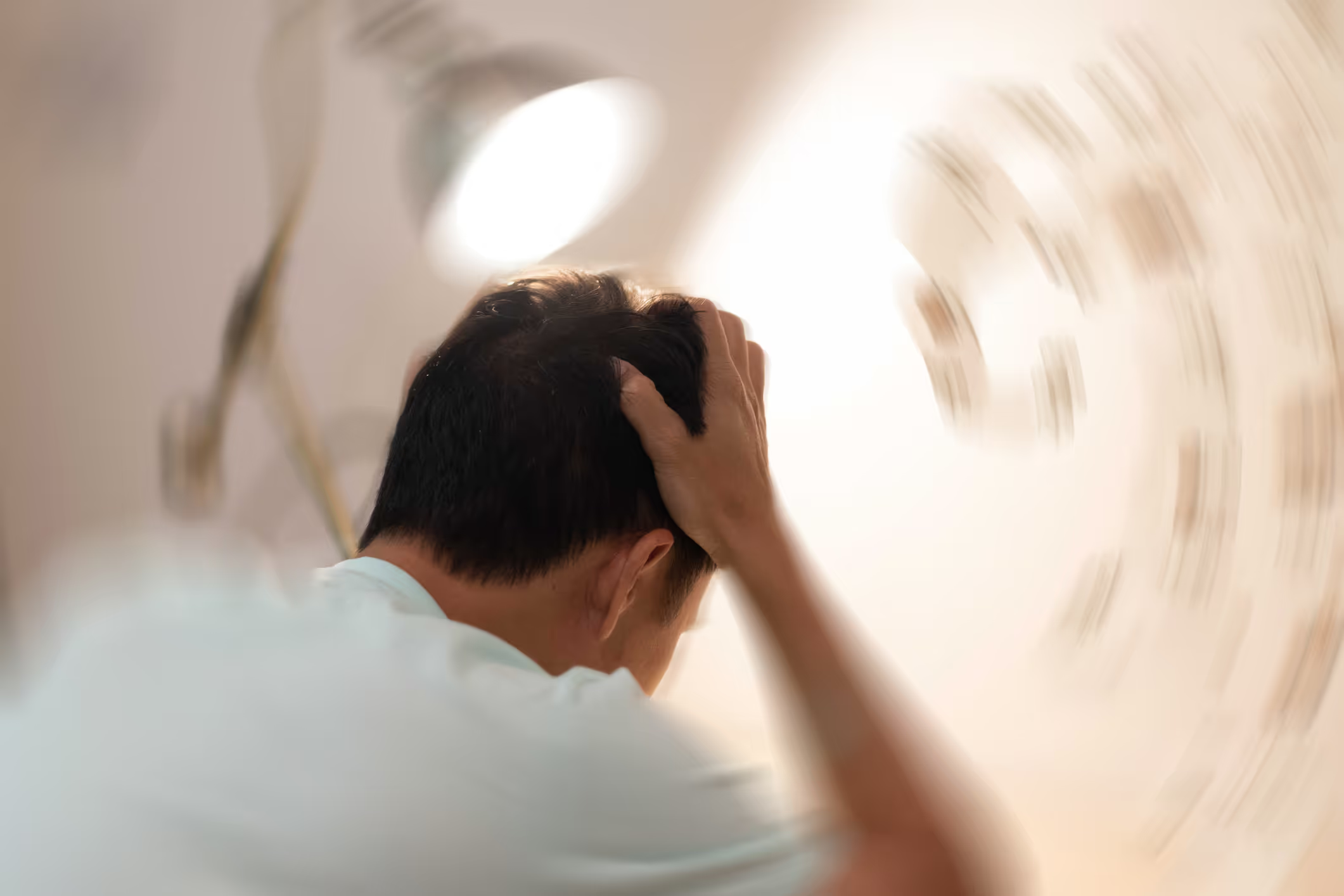
BPPV, benign positional paroxysmal vertigo, is a form of positional vertigo. This means that dizziness is triggered when you change the position of your head. For example, when you turn over in bed, stand up from lying to sitting or lying down, bend forward to put on shoes, or bend your head backwards to look for something. BPPV is the most common form of dizziness that 20% of us will experience one or more times in our lifetime. But BPPV is also one of the easiest to treat if examined and treated by a competent healthcare professional. Between 70-90% of those with the most common type of BPPV in the posterior arch, canalolithiasis, become completely free of dizziness after 1-3 treatments with repositioning maneuvers. However, studies also show that up to 12% suffer from persistent positional dizziness even after treatment with traditional repositioning maneuvers. People in this group often have other diseases as well. These include metabolic problems, menopause, diabetes, high cholesterol, migraines or head trauma such as a traffic accident or fall.
Paradoxically, cholesterol-lowering, pain-relieving and migraine medications can also cause chronic BPPV. Research shows that several medications make us more prone to developing BPPV and persistent BPPV. These include antidepressants, drugs that affect the central nervous system such as neurotin, or drugs that suppress the production of stomach acid. In such cases, it is of course important to weigh up the reason for using the medication and its side effects. It is important to have a thorough review of the medication with your GP to find out if the medication may be the cause of chronic BPPV. In many cases, these are life-saving medications that must be used, or medications that relieve other more serious or debilitating symptoms than dizziness caused by BPPV.
Multi-channel BPPV, BPPV in multiple archways at the same time, is also often the cause of persistent and chronic BPPV. Even without regular use of medication, metabolic problems or any of the other above-mentioned risks of chronic BPPV.
Whatever the cause of chronic BPPV, they have in common that the particles in the balance organ of the inner ear continuously loosen and stray into the semicircular canals and stick to the motion sensors (cupula), BPPV cupulolithiasis.
Treatment of chronic BPPV:
As the underlying cause of chronic BPPV differs from individual to individual, it is important to do a thorough and comprehensive examination to map all symptoms and complaints, challenging all parts of the balance and sensory system to identify which parts of the brain and nervous system need rehabilitation in addition to repositioning treatment of BPPV. In most cases, regardless of the cause of chronic dizziness, research shows that one can alleviate and reduce the intensity of dizziness using neurological rehabilitation and vestibular rehabilitation therapy. Research also shows that TRV chair treatment can have a significantly better effect than traditional repositioning maneuvers. The reason for this is that multiple archways can be treated simultaneously using the TRV chair, and the TRV chair creates a better acceleration momentum in the fluid inside the semi-circular canals and therefore pulls the particles along in a better way that is not possible with traditional maneuvers.
Brain Camp is one of the few clinics in Europe that can offer the combination of tailored neurological rehabilitation and treatment of BPPV using the TRV Chair.
The TRV chair is designed to rotate the patient 360 degrees in multiple planes, creating acceleration of the fluid in the archways to "shake" the particles loose more effectively than traditional maneuvers. Research shows that the treatment of BPPV in a TRV chair can have a significantly better effect and is more gentle for patients who have difficulties with the more traditional treatment methods due to, for example, neck injuries. Treatment using the TRV chair has been shown to be particularly effective for those with chronic BPPV and frequent relapses, and for those with BPPV in multiple arches. It has also been shown that treatment using a TRV chair can reduce the risk of recurrence or reduce the frequency of recurrence.
In our experience, most patients with chronic BPPV, regardless of the cause, benefit best from a combination of tailored neurological rehabilitation, regular repositioning treatment in a TRV chair with weeks or months between each treatment, and thorough training on how to reposition themselves 1-3 times a week.
If you are taking any of the above medications, it is important to have a thorough review of the medication with the prescribing doctor to assess whether it may be appropriate to try other medications that may have less of an impact on BPPV. However, as mentioned earlier, in many cases there are life-saving medications that must be used, or medications that relieve other more severe or debilitating symptoms than dizziness caused by BPPV. One must then adapt neurological rehabilitation, repositioning treatment in a TRV chair, and repositioning maneuvers that one does at home, based on the frequency and intensity of recurrence of BPPV dizziness.
BrainCamp has extensive experience in the treatment and rehabilitation of patients with chronic BPPV. Our first examination is a thorough and comprehensive functional neurological examination that lasts about 5 hours. This examination identifies which parts of the balance system, sensory system, and other parts of the brain and nervous system have challenges and need rehabilitation. We use the details of this examination to best tailor the first phase of rehabilitation. This examination includes video nystagmography that analyzes purposeful eye movements to see how different parts of the brain and nervous system function, computerized balance measurement, tests that challenge different parts of the coordination system, and various tests specific to different forms of dizziness. Including the Dix-Hallpike test with video-oculography which is the standard test for BPPV. Video-oculography is an examination with a mask that has an infrared camera attached to analyze nystagmus caused by BPPV. Video-oculography is important for more precise analysis of the direction of the nystagmus and how long the nystagmus lasts. This information tells us which archway has BPPV and what form of BPPV the patient has. This is essential, as the different archways and forms of BPPV require different treatment.
This video gives you an introduction to what your first examination at Brain Camp will include.
References:
- American Hearing research foundation.
- Abdul Kader Afif Yamout, 2022. Comparison of the effectiveness of TRV chair and canalith repositioning procedure (VRP) for the treatment of benign positional paroxysmal positional vertigo (BPPV). International journal of otolaryngology and head & neck surgery, 2022, 11, 143-153.
- Balanselaboratoriet.no
- Berit Hackenberg et al, 2023. Vertigo and its burden of disease-Results from a population-based study. Laryngoscope Investigative Otolaryngology. 2023.
- Bhattacharyya N, et al. 2008. Clinical practice guideline: benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2008.
- Dimitris G, et al. 2011. Diagnosis of single- or Multiple-Canal benign paroxysmal positional vertigo according to the type of nystagmus. International Journal of Otolaryngology, vol 2011, page 13, 2011.
- Giuseppe Chiarella, wt al, 2017. Hashimoto thyroiditis and vestibular dysfunction. Endocrine practice 2017; 23: 7: 863-868.
- Gordon CR, et al. 2004. Is posttraumatic benign paroxysmal positional vertigo different from the idiopathic form?. Arch Neurol. 2004.
- Gordon CR, et al. 2005. Benign paroxysmal positional vertigo: who can diagnose it, how should it be treated and where? Harefua. 2005.
- Hansen S, Kalberg M. Benign ataropksysmal positional vertigo- the most frequent form of otogenic vertigo. Ugeskr Læger 2007; 169: 1996-2002.
- Crystal Sickness.com
- Lopez-Escamez JA, et al. 2003. Impact of treatment on health-related quality of life in patients with posterior canal paroxysmal positional vertigo. Otol Neurotol. 2003.
- Lopez-Escamez JA, et al. 2005. Long-term outcome and health-related quality of life in benign paroxysmal positional vertigo. Eur Arch Otorhinolaryngol. 2005.
- Manzani D, et al. 2006. Life events and benign paroxysmal positional vertigo: a case-controlled study. Acta Otolaryngo. 2006.
- Mohammad Abu Shaphe et al, 2023. Effectiveness of Epley-Canalith Repositioning Procedure versus Vestibular Rehabilitation Therapy in Diabetic Patients with Posterior Benign Paroxysmal Positional Vertigo: A Randomized Trial. Life 2023;13: 1169.
- M von Brevern, et al. 2006. Epidemiology of benign paroxysmal positional vertigo: a population based study. Journal of Neurology, Neurosurgery & Psychiatry 2007; 78: 710-715.
- Niels West et al, 2015. Repositioning chairs in benign paroxysmal positional vertigo: implication and clinical outcome. European Archives of Otorhinolaryngology
- Pollak, et al. 2002. Effectivness of the particle repositioning maneuver in benign paroxysmal positional vertigo with and without additional vestibular pathology. Oto Neurotol. 2002.
- Salvinelli F, et al. 2003. Benign paroxysmal positional vertigo: a comparative prospective study on the efficacy of Semont´s maneuver and no trewatment strategy. Clin Ter. 2003.
- Salvinelli F, et al. 2004. Benign paroxysmal positional vertigo: diagnosis and treatment. Clin Ter. 2004.
- Seong Jun Choi et al, 2012. Clinical features of recurrent or persistent benign positional paroxysmal positional vertigo. Journal of otolaryngology-head and neck surgery. 2012.
- Serkan Abdulovski and Mads Klokker, 2021, Repositioning chairs in the diagnosis and treatment of benign paroxysmal positional vertigo- A systematic review. The journal of international advanced otology 2021; 17 (4): 353-360.
- Sertac Yetiser, 2019. Review of the pathology underlying benign paroxysmal positional vertigo. Journal of international medical research 2019; 48(4): 1-12.
- T. D. Fife, et al. 2008. Practice Parameter: Therapies for benign paroxysmal positional vertigo (an evidence-based review): Report pf the quality standard subcommittee of the American Academy of Neurology. Neurology, 2008.
- Yuanjia Hu et al, 2023. Global research trends in benign paraoxysmal positional vertigo: a bibliometric analysis. Frontier. 2023

