Concussion - What happens to the brain? PART 2

As we started with in Part 1 of this article, research shows that the primary functional disorders caused by a concussion produce a domino effect of functional disorders in both external (cortical) and internal (subcortical) parts of the brain. Including parts of the brain involved in processing and coordinating multiple sensory impressions simultaneously (multisensory integration), which are responsible for synchronizing the activation of several different centers with different properties in the brain simultaneously to perform both physical and cognitive tasks (cross-modal activation), while both cortical and subcortical areas that are not normally activated during certain tasks are activated in people who have suffered a concussion and mild traumatic brain injury. Research has shown that disrupted synchronization between the brain's reception of sensory information and production of motor signals results in impaired neuroplasticity and learning. This is one of the reasons why it is difficult to find effective treatments that can reduce symptoms and improve quality of life in children and adults with chronic concussion syndrome, post-concussion syndrome.
Function and dysfunction in the outer and inner parts of the brain.
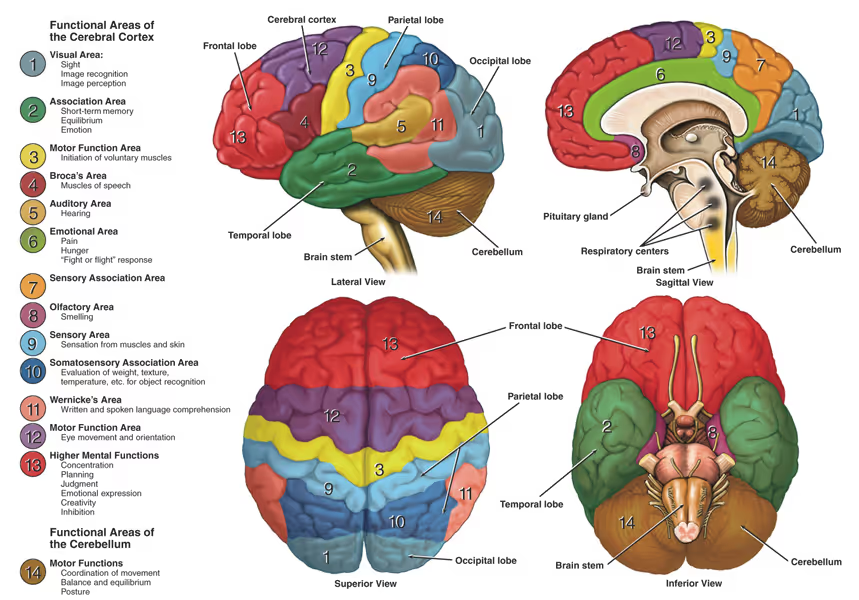
To get a better understanding of what happens in the brain in a concussion and what causes the broad symptom burden of concussion and post-concussion syndrome, we need to review the functions of some of the areas of the brain and what happens to them in a head trauma. It is not so important to remember or understand all the details in this review, but we need to review these areas of the brain and their functions to get a better understanding of the "big picture" of what happens to the brain in a concussion and why post-concussion syndrome causes such a broad symptom burden.
Superiorcolliculus
The superior colliculus is an important structure in the brainstem for processing and coordinating different sensory impressions simultaneously (multisensory integration), and is important for providing synchronized activation of several different centers with different properties in the brain simultaneously to perform both physical and cognitive actions (cross-modal communication). In people with post-commotio syndrome, research shows that there is a reduced response in the superior colliculus, leading to disruption in how the brain coordinates and integrates visual information, movement information from muscles and joints, movement information from the balance organ in the inner ear, and auditory information such as language and sounds from our environment. This interferes with functions that affect motor skills, orientation, concentration and attention.
The superior colliculus also has important functions involved in gaze control and fine motor control of purposeful eye movements. Impaired function in the superior colliculus can thus also make it more challenging to orientate visually, and more challenging and exhausting to do concentration work that strains the gaze, including reading.
Corpus callosum
The corpus callosum is the largest collection of nerve fibers connecting the right and left hemispheres of the brain and plays a central role in communication between these two hemispheres. These nerve fibers act as communication bridges, transmitting information between the two hemispheres, enabling coordinated and integrated functioning of the cerebral hemispheres. Research from 2019 using diffusion tensor imaging (DTI) shows that people with chronic concussion syndrome, post-concussion syndrome, have disrupted connections and integrity in the corpus callosum. These dysfunctions contribute to reduced cognitive performance, among other things. Especially in working memory, attention and processing speed.
Prefrontal cortex
The prefrontal cortex has important functions involved in ensuring good cognitive abilities, decision-making and working memory. The prefrontal cortex also communicates with parts of the brain that control motor function and collects various sensory inputs that are important for planning, organizing, initiating and coordinating complex movements involving multiple body parts and sensory systems. Including primary motor cortex, premotor cortex, supplementary motor area, primary and secondary visual areas, posterior parietal cortex, somatosensory cortex, and the vestibular cortex. Good function in the prefrontal cortex and good communication with the other areas of the brain is essential for, among other things, smooth and effortless eye-hand and eye-foot coordination, adapting motor movements and reactions to changes in the environment, and being able to perform motor movements while facing cognitive challenges.
In people with post-commotio syndrome, there is evidence of reduced activity in the prefrontal cortex and disrupted communication with other areas of the brain. This contributes to concentration difficulties, impaired cognitive function, reduced responsiveness and precision in complex motor challenges such as eye-hand coordination and multitasking in motor challenges.
Superior parietal cortex
The superior parietal cortex is involved in important functions of integrating sensory information (including movement information from joints and muscles, and the balance organ in the inner ear), providing good spatial and movement orientation, and maintaining good attention. All these functions are important to ensure good and effortless motor and movement skills, and cognitive and executive abilities.
Good communication between the superior parietal cortex and, among others, primary motor cortex, premotor cortex and supplementary motor areas, frontal eye fields, primary and secondary somatosensory cortex, temporoparietal and vestibular cortex is important for smooth and controlled conscious movements with the body, planning and coordination of complex and sequential motor actions, fine motor control over purposeful eye movements and aligning purposeful eye movements with movements of other body parts, higher cognitive functions such as decision-making and understanding the intentions and beliefs of others, and orientation over movement and space.
- Primary motor cortex is mainly responsible for the execution of conscious motor movements.
- The premotor cortex and supplementary motor area are involved in planning and coordinating more complex, sequential motor actions.
- The frontal eye field is involved in controlling eye movements, which are critical for visual attention and eye-hand coordination.
- The prefrontal cortex is important for higher cognitive functions such as decision-making, working memory and attention control.
- Primary and secondary somatosensory cortex are responsible for processing information about touch, pressure, pain, temperature and body position (proprioception), all of which are critical for motor control.
- The temporoparietal junction (TPJ) is involved in several aspects of cognition, including theory of mind (understanding the intentions and beliefs of others), attention and spatial processing.
Several studies show that concussion can lead to activity disturbances and changes in connectivity in the superior parietal cortex in patients with post-concussion syndrome. These functional disturbances in the superior parietal cortex can contribute to, among other things, impaired balance and coordination, impaired fine motor control over complex motor movements with the body and other body parts, impaired fine motor control and coordination of purposeful eye movements that are important for reading and visual orientation, difficulties with higher cognitive challenges, and difficulties with spatial orientation.
Temporal cortex
The temporal cortex plays a key role in processing and understanding visual and auditory information, but its role in processing movement signals from the balance organ in the inner ear and from joints and muscles is less direct and more complex. Temporal cortex receives:
- Visual information: Parts of the temporal cortex, particularly those areas known as the ventral stream or "what" pathway, are involved in object recognition and face recognition.
- Auditory information: The temporal gyrus contains primary and secondary auditory cortexes, which process and interpret sounds.
- Vestibular information (movement information from the balance organ in the inner ear): Although the vestibular system primarily sends information to areas such as the parietal cortex, thalamus and cerebellum, the temporal cortex can become involved in more complex movement challenges and integration of this movement information. Especially in connection with memory and spatial orientation.
- Proprioceptive information (movement information from joints and muscles): Proprioception, or the perception of body position and movement, is mainly processed by areas such as the atosensory cortex and cerebellum. Similar to vestibular information, the temporal cortex can be involved in complex movement challenges and integration of this information, especially in relation to memory and spatial orientation.
While the temporal cortex directly processes visual and auditory information, this area also has important functions involved in processing, coordinating and interpreting movement information from the balance organ in the inner ear and movement information from joints and muscles in complex movement challenges that also require cognition. For example, when walking in rough terrain and you have to be visually alert and plan movements before executing them, while at the same time being able to stop initiated movements in the event of unforeseen dangerous terrain. And eye-hand and eye-foot coordination, which also challenges concentration and impulse control at the same time. For example, catching a ball with your hands or feet, or writing while concentrating to retain the content of a meeting or lecture.
The temporal cortex also has important roles in our memory. Both visual and auditory memory.
- Visual memory: Temporal cortex, particularly structures in the medial-temporal lobe such as the hippocampus and surrounding areas, are important for the formation and integration of visual memory. When we perceive visual information, such as objects, faces or surroundings, it undergoes initial processing in the primary visual cortex and then moves on to areas for more complex processing and understanding of visual impressions, including the temporal cortex. Within the temporal cortex, there are specialized regions, such as the inferotemporal cortex, that process and analyze complex visual stimuli. These areas are responsible for recognizing and storing visual features, such as shape, color, texture and spatial relationships. For example, the temporal cortex helps identify familiar faces, objects and places. Furthermore, the connections between the temporal cortex and the hippocampus are crucial for systematizing and integrating visual memories. The hippocampus receives processed visual information from the temporal cortex and integrates it with other situational details to form episodic memories. These memories are the retrieval of specific events or experiences associated with visual stimuli.
- Auditory memory: Similar to visual memory, the temporal cortex is involved in processing auditory memory. Primary auditory cortex, located within the temporal cortex, receives sound information from the ears and performs initial processing, such as frequency and intensity analysis. As the auditory information travels through the auditory pathway, it reaches higher auditory areas in the temporal cortex. Within the temporal cortex, there are specialized regions, such as the superior temporal gyrus, that are involved in complex auditory processing and memory formation. These areas help with the recognition and storage of auditory features, such as pitch, rhythm, timbre and language comprehension. For example, the temporal cortex helps recognize familiar voices or melodies. Furthermore, the connections between the temporal cortex and the hippocampus play an important role in the formation of auditory memories. The hippocampus integrates the processed auditory information from the temporal cortex with other relevant contextual details, such as emotional meaning or associated events, to form episodic memories.
In summary, the temporal cortex, along with its specialized areas and connections to the hippocampus, among others, is essential for the processing, recognition and storage of visual and auditory memory. It enables us to perceive, recognize and remember complex visual stimuli and auditory information, allowing us to form detailed and meaningful memories of the world around us. At the same time, the temporal cortex also has important functions involved in processing, correlating and interpreting movement information from the balance organ in the inner ear and movement information from joints and muscles in complex movement challenges that also require cognition. Research shows functional disturbances and reduced connectivity in the temporal cortex in people with chronic concussion syndrome. This impaired connectivity and dysfunction contributes to a wide range of symptoms. Including impaired concentration and memory, and impaired balance, coordination, orientation ability in more complex movement challenges that include motor and cognitive skills.
Vestibular cortex
The vestibular cortex is distributed over several areas of the brain, including the parietal and temporal cortex and interconnected with a large network involved in spatial attention and sensorimotor control of eye and body movement.
The vestibular cortex integrates information from the balance organ in the inner ear with information from other sensory systems (such as visual information and movement information from joints and muscles) to create a coherent perception of the body's position and movement in space. This helps to coordinate eye and head movements, postural control, and is important for maintaining balance and stability. As mentioned above, the vestibular cortex also plays a key role in visuospatial attention and awareness of the body's position in space.
As mentioned, the vestibular cortex also has connections and communicates with several other parts of the brain that are both involved and not involved in balance and physical orientation. Including the thalamus, cerebellum, visual cortex, somatosensory cortex, hippocampus and prefrontal cortex. The connections between the vestibular cortex and these other parts of the brain play a crucial role in a wide range of functions. Not only related to balance and coordination, spatial orientation, and navigation. But also functions related to both cognition and memory.
- The thalamus relays vestibular information to the cortex and is crucial for conscious perception of vestibular stimuli well balance the organ of the inner ear.
- The cerebellum helps fine-tune motor commands and improve coordination, especially those related to balance. Its connection to the vestibular system is crucial for maintaining balance, orination and adapting movements.
- The visual cortex and the vestibular system work together to help maintain balance and spatial orientation. For example, when you move your head, your eyes automatically adjust to keep your gaze stable at a point so that you experience being in a wading position, perceiving your surroundings as they are whether objects are moving or stationary. This is partly a result of the vestibulo-ocular reflex (VOR) and cervico-ocular reflex (COR), mechanisms where movement signals from the balance organ in the inner ear and movement information from joints and muscles in the neck communicate with the visual system.
- The somatosensory c ortex communicates with the vestibular cortex to help integrate movement information from joints and muscles, and touch stimuli. For example, when walking, muscles and joints send movement information about the positions of the legs and touch sensors in the skin sense the surface you are walking on, providing additional information about the spatial conditions.
- The hippocampus is known for its role in memory and spatial navigation. Interaction with the vestibular system can support the creation of cognitive maps, which are mental representations of the layout of environments.
- The prefrontal cortex's connections with the vestibular cortex play a role in how the brain uses vestibular information for higher-level functions such as planning and decision-making. The prefrontal cortex is involved in higher cognitive functions such as decision-making, problem solving, planning and self-control, receiving information from the vestibular cortex and other sensory areas to form a holistic understanding of body position and movement. Through this communication, the prefrontal cortex can help plan and adapt motor actions based on the body's balance and spatial orientation. This interaction between the prefrontal cortex and vestibular cortex is important for maintaining balance and controlling body movements in different situations and environments.
It is well known that patients with chronic concussion syndrome are often plagued with dizziness as a result of disturbed function of the vestibular system. This includes damage to the balance organ in the inner ear, impaired connectivity, impaired integration of balance signals from the balance organ in the inner ear, and impaired communication with other connecting areas in the brain. Recent research also suggests that the dysfunction of the vestibular cortex and disruptions in its communication with other areas of the brain contribute to increased challenges with both cognitive and executive functions in people with chronic concussion syndrome.
Cerebellum
The cerebellum has traditionally been primarily associated with the coordination of motor movements, balance and equilibrium. New research has also begun to uncover the extensive roles of the cerebellum, extending its functions to involvement in cognition and emotion.
The known main role of the cerebellum lies in the coordination of motor activities, especially purposeful movements of the body, arms and legs, and eyes. The cerebellum does this by receiving input from sensory systems and different parts of the brain involved in motor control, integrating this input, and fine-tuning motor commands to the muscles. This precise coordination enables smooth, purposeful movements and ensures balance and posture.
The integral role of the cerebellum in motor control is demonstrated when damage to the cerebellum occurs. This results in ataxia, a condition characterized by loss of full control over body movements, leading to abnormal gait, poor coordination and unsteady movements.
Recent research is beginning to provide a deepened understanding of the role of the cerebellum extended to include various non-motor functions, including in cognition. The cerebellum is involved in several cognitive processes such as attention, language, working memory and visual-spatial perception. It is believed that the cerebellum supports these cognitive functions by maintaining the timing and accuracy of mental processes, in the same way as it does with motor movements and actions.
Research also links the cerebellum to emotional processing. Through its connections with areas called the amygdala, hypothalamus and prefrontal cortex. All key regions involved in emotion, the cerebellum appears to contribute to the regulation of affective responses.
Damage to the cerebellum has been associated with changes in personality and mood, including affect flattening or disinhibited and inappropriate behavior. This highlights the role of the cerebellum in modulating our emotional responses.
New research shows that people with post-commotio syndrome have reduced activity and connectivity in the cerebellum, which can contribute not only to motor challenges and impaired coordination. But also cognitive and emotional challenges.
Executive summary
The description and understanding of these areas of the brain illustrates how each individual function of our brain and nervous system does not work in isolation, but instead deeply and complexly integrate with each other to create a wide range of motor, cognitive, executive and emotional functions. This also explains why we see a broad domino effect of secondary dysfunctions resulting from the primary cortical (external) and subcortical (internal) dysfunctions caused by a concussion and post-concussion syndrome. This new knowledge and understanding of what happens in the brain also gives us a better understanding of why many people with concussion and post-concussion syndrome experience such a broad and complex spectrum of disabling symptoms and reduced quality of life.
At Brain Camp, we therefore see the need for a broad and comprehensive functional examination of the brain and nervous system to identify which parts of the brain and nervous system need rehabilitation. This includes tests that challenge balance and coordination, physical and cognitive responsiveness, fine motor control over purposeful eye movements, and the brain's awareness of movement with the neck, back, and arms and legs.
We place great emphasis on several tests, but some of the most important tests we do are computer-based video nystagmography, which measures fine motor control over purposeful eye movements. The reason we place so much emphasis on these tests is that research shows that impaired fine motor control and coordination of purposeful eye movements may be one of the main reasons why children and adults with post-commotio syndrome suffer from fatigue and brain fog, difficulties with reading and concentration, difficulties processing and filtering visual impressions, and reduced tolerance to physical activity.

Thereis hope for improvement
Even if you have been suffering from symptoms due to post-commotio syndrome for several years and have not responded to previous treatment, recent research shows that there is hope of reducing the intensity of symptoms and improving quality of life with the help of tailored neurological rehabilitation. We at Brain Camp, Kim Tore Johansen and his team, have long and broad experience with patients of all ages with post-commotio syndrome and will do our utmost to help you towards a better everyday life.
Reference list:
1. badre, D., & Frank, M. J. (2020). Interactions between prefrontal cortex and basal ganglia during decision making. Nature Reviews Neuroscience, 21(12), 691-705.
2 Bertolini, G., & Tarnutzer, A. A. (2020). The neural basis of spatial orientation and its modulation by multisensory and vestibular input. Journal of Neurophysiology, 124(3), 738-751.
3. betzel, R. F., Medaglia, J. D., & Bassett, D. S. (2020). Diversity of meso-scale architecture in human and non-human connectomes. Nature Communications, 11(1), 1-13. This study explores the organization of "small world" networks in human
4 Buki A, Egyud L, Okonkwo DO, et al. Update on mild traumatic brain injury: an introduction to diagnosis and management. J Neurol Neurosurg Psychiatry. 2021;92(2):219-227. doi:10.1136/jnnp-2020-323628
5 Cai, Y., et al. "Decreased functional connectivity density in subjects with post-concussion syndrome." Frontiers in neurology 9 (2018): 572.
6 Chen, J. K., et al. "A prospective study of white matter abnormalities in mild traumatic brain injury at the acute stage." Neurology 89.15 (2017): 1562-1571.
7 Davenport, N. D., et al. "Abnormalities in visual and auditory cortical activation in mild traumatic brain injury." Journal of the International Neuropsychological Society 25.1 (2019): 26-37.
8 De Beaumont L, Tremblay S, Lassonde M, Théoret H. Long-term and cumulative effects of sports concussion on motor cortex inhibition. Neurosurgery. 2021;89(Suppl_1):S34-S42. doi:10.1093/neuros/nyaa527
9 Delaney, J. S., et al. "Balance and vestibular dysfunction in individuals with persistent post-concussion syndrome." Journal of head trauma rehabilitation 34.4 (2019): E28-E36.
10 Faghri PD, Rodrigues E, Lo CK, Yost RA. Virtual reality-based cognitive-motor rehabilitation in persons with traumatic brain injury: a pilot study. Am J Phys Med Rehabil. 2020;99(6):515-522. doi:10.1097/PHM.0000000000001398
11. Figueiredo, T. H., et al. "Altered resting-state connectivity in post-concussion syndrome: a pilot study." Brain Injury 33.1 (2019): 114-121.
12 Frederick R. Carrick et al, 2012. Whole body rotation omitting a multi-axial rotational chair in case of multiple system atrophy-like syndrome. Functional Neurology, Rehabilitaiton and Ergonomics. Vol 2, No 1, 2012.
13. Frederick R. Carrick wt al, 2011, The effect of whole body rotations in the pitch and yaw planes on postural stability. Functional Neurology, Rehabilitaiton and Ergonomics. Vol 2, 167-179, 2011.
14 Frederick R. Carrick et al, 2015. Evaluation of the effectiveness of novel brain and vestibular rehabilitation treatment modality in PSTD patients who have suffered combat-related traumatic brain injuries. Frontiers in Public Health vol 3 (2015), article 15.
15 Frederick R. Carrick et al, 2015. Short- and long-term effectiveness of a subject's specific novel brain and vestibular rehabilitation treatment modality in combat veterans suffering PTSD. Frontiers in Public Health vol 3 (2015), article 151.
16. furlan, L., & Krüger, O. (2020). Involvement of the human ventromedial prefrontal cortex in goal-directed motor planning. eLife, 9, e57737.
17 Giza CC, Hovda DA. The new neurometabolic cascade of concussion. Neurosurgery. 2021;89(Suppl_1):S24-S33. doi:10.1093/neuros/nyaa523
18 Guo, Z., Li, A., & Yu, L. (2020). Neural mechanisms underlying the integration of situational information into attribution outcomes. Human Brain Mapping, 41(6), 1506-1518.
19. Directorate of Health
20. hilgetag, C. C., & Goulas, A. (2020). Is the brain really a small-world network?. Brain Structure and Function, 225(2), 647-660.
21 Hoffman, N. L., et al. "Vestibular dysfunction in post-concussive syndrome." Journal of neurologic physical therapy: JNPT 43.4 (2019): 214-221.
22 Huang C, Duan K, Hu S, et al. Dysregulation of the immune system in post-concussion syndrome. Front Neurol. 2021;12:676727. doi:10.3389/fneur.2021.676727
23 Jeannie Ponsford et al, 1999. Cognitive and Behavioral Outcome Following Mild Traumatic Head Injury in Children. Journal of Head Trauma Rehabilitation, August 1999.
24 Kheradmand, A., & Winnick, A. (2020). Vestibular control of standing balance is enhanced with increased cognitive load. Frontiers in Neurology, 11, 566.
25 Kim, Y. W., et al. "Altered cortical thickness in patients with post-concussion syndrome: a structural magnetic resonance imaging study." Journal of Neurotrauma 36.2 (2019): 306-312.
26. kim, H. E., Morehead, J. R., Parvin, D. E., Moazzezi, R., & Ivry, R. B. (2020). Inhibition of saccades elicits attentional suppression and retinotopic adaptation in human visual cortex. Journal of Neuroscience, 40(14), 2889-2901.
27 King, L. A., et al. "Persistent symptoms and activity changes three months after mild traumatic brain injury." Journal of rehabilitation research and development 55.3 (2018): 305-314.
28. kromrey, S., Haarmeier, T., & Thier, P. (2020). Neural basis of the saccadic suppression of displacement detection. Cerebral Cortex, 30(6), 3586-3598.
29 Kumar, A., et al. "Alterations in functional connectivity of small-world brain networks in patients with mild traumatic brain injury." PloS one 13.10 (2018): e0205549.
30 Leddy, J.J., Haider, M.N., Ellis, M.J., et al. (2021). "Early Subthreshold Aerobic Exercise for Sport-Related Concussion: A Randomized Clinical Trial." Journal of Neurotrauma, 38(4), 479-487.
31 Leddy, J.J., Haider, M.N., Hinds, A., et al. (2022). "Early Exercise After Sport-Related Concussion: A Systematic Review and Meta-Analysis." British Journal of Sports Medicine, 56(4), 192-197.
32 Leddy, J. J., et al. "A preliminary study of the effect of early aerobic exercise treatment for sport-related concussion in males." Clinical Journal of Sport Medicine 28.1 (2018): 13-21.
33 Mannix R, Meehan WP, Monuteaux MC, et al. Clinical predictors of prolonged recovery after concussion in children and adolescents. JAMA Pediatrics. 2020;174(2):e195905. doi:10.1001/jamapediatrics.2019.5905
34 Mark E. Halstead et al, 2010. Sport-Related Concussion in Children and Adolescents. Pediatrics volume 126, number 3, September 2010.
35 Matthew T. Neal et al, 2011. Concussions: What a neurosurgeon should know about current scientific evidence and management strategies. Surgical Neurology International 2012; 3:16.
36 Maugans TA, Farley C, Altaye M, Leach J, Cecil KM. Pediatric sports-related concussion produces cerebral blood flow alterations. Pediatrics. 2020;146(2):e20193980. doi:10.1542/peds.2019-3980
37 McCrea, M., Meier, T., Huber, D., et al. (2020). "Role of Advanced Imaging in Sport-Related Concussion." Journal of Head Trauma Rehabilitation, 35(1), 1-8.
38 McDougle, S. D., & Taylor, J. A. (2020). Dissociable cognitive strategies for sensorimotor learning. Nature Communications, 11(1), 1-13.
39 Meier TB, Karr JE, Karr JW, et al. Mild traumatic brain injury in the United States military: epidemiology, risk factors, and mitigation strategies. Curr Opin Neurol. 2021;34(6):709-714.
40. niv, Y., & Langdon, A. (2021). Reinforcement learning with continuous actions through model-based planning. Journal of Neuroscience, 41(1), 5-15.
41 Norwegian Health Information, Norwegian patient handbook.
42 Patel R, Sampaio-Baptista C, Johansen-Berg H. Structural and functional plasticity following concussion. Neurosci Lett. 2020;725:134902. doi:10.1016/j.neulet.2020.134902
43 Perrault, T. J., et al. "Superior colliculus neuronal responses to multisensory stimuli in post-concussive syndrome." Journal of Neurotrauma 36.5 (2019): 791-802.
44. salari, E., Bütefisch, C. M., & Zimerman, M. (2020). Investigating the neural basis of theta burst stimulation to premotor cortex on emotional facial expression recognition: role of the mirror neuron system. Scientific Reports, 10(1), 1-10.
45 Schneider, K.J., Meeuwisse, W.H., Nettel-Aguirre, A., et al. (2023). "Rest and Return to Activity After Sport-Related Concussion: A Systematic Review and Meta-analysis." British Journal of Sports Medicine, 57(1), 3-8.
46 Seabury, S. A., et al. "Neuroimaging correlates and predictors of symptom improvement following concussion in a pediatric population." Journal of Neurotrauma 36.22 (2019): 3182-3192.
47 Schneiderman, A. I., et al. "Relationship between history of traumatic brain injury and recent risky driving behavior: a population-based study." The Journal of the American Medical Association 296.9 (2006): 2574-2581.
48 Shahim, P., et al. "Multimodal assessment of neurodegeneration in post-concussion syndrome after mild traumatic brain injury: a prospective longitudinal study." Journal of Neurology, Neurosurgery & Psychiatry 91.3 (2020): 265-276.
49 Shumskaya E, Andriessen TMJC, Norris DG, Vos PE. Abnormal neuronal activation after concussion in the absence of structural abnormalities on conventional neuroimaging. J Neurol Neurosurg Psychiatry. 2021;92(2):170-177. doi:10.1136/jnnp-2020-323558.
50 Shumskaya, E., et al. "Diffuse white matter abnormalities in chronic mild traumatic brain injury and their relationship to neuropsychological functioning." NeuroImage: Clinical 21 (2019): 101632.
51 Smith, P. F., & Zheng, Y. (2020). From ear to uncertainty: vestibular contributions to cognitive function. Frontiers in Integrative Neuroscience, 14, 4.
52 Snellman M, Ramberg E, Lindqvist J, et al. Genetic variation associated with concussion susceptibility in Swedish ice hockey players. PLoS One. 2021;16(2):e0247558. doi:10.1371/journal.pone.0247558
53 Timothy Belton and Robert A. McCrea (2000). Role of the Cerebellar Flocculus Region in Cancellation of the VOR During Passive Whole body Rotation. Journal of Neurophysiology, 84: 1599-1613, 2000.
54 Tremblay, S., & Small, S. L. (2020). Motor learning and the covert practice of movement. Journal of Neuroscience, 40(50), 9552-9560.
55. van der Horn, H. J., et al. "Structural connectivity changes in post-concussion syndrome: a diffusion tensor imaging study." NeuroImage: Clinical 22 (2019): 101707.
56 Wu, Y., et al. "Cerebellar gray matter reductions associate with decreased functional connectivity in the vestibular cerebellum in patients with persistent postural-perceptual dizziness." Journal of Neurology 266.8 (2019): 1993-2003.
57 Y.P. Ivanenko et al, 1997. The contribution of otoliths and semicicular canals to the perception of two-dimensional passive whole-body motion in humans. Journal of physiology, 502. 1, pp. 223-233, 1997.
58 Yuh EL, Mukherjee P, Lingsma HF, et al. Magnetic resonance imaging improves 3-month outcome prediction in mild traumatic brain injury. Ann Neurol. 2021;89(1):49-59. doi:10.1002/ana.25920
59 Yuan, W., et al. "Functional connectivity changes in mild traumatic brain injury assessed using resting-state functional magnetic resonance imaging." The Journal of Neuropsychiatry and Clinical Neurosciences 31.1 (2019): 47-53.
60 Zatorre, R. J., & Fields, R. D. (2020). Neuroscience: Can musical training change the brain?. Current Biology, 30(13), R722-R724.
61 Zhou, Y., et al. "EEG source imaging correlates of mild traumatic brain injury recovery trajectories." Brain 142.3 (2019): 633-646.
62. zhu, D. C., et al. "Altered resting state connectivity in persistent post-concussive symptoms following mild traumatic brain injury: a network analysis." NeuroImage: Clinical 20 (2018): 18-27.
63 Zu Eulenburg, P., & zu Eulenburg, C. (2020). Cortical networks of the human vestibular cortex: Evidence from structural and functional connectivity studies. Brain Structure and Function, 225(3), 801-814.