Concussion - What happens to the brain? PART 1
Every year, more than 600 people per 100,000 suffer a concussion, commotio cerebri. The concussion occurs as a result of a direct or indirect impact to the head that causes the brain to experience an acceleration force and shake inside the head. This "brain shaking" causes physical tensile damage to the nerves that triggers several biochemical reactions. The tensile damage and biochemical reactions result in immediate functional disturbances, including something called excitotoxicity. Excitotoxicity is a reaction following damage to nerve cells where there is a leakage of substances dedicated to, among other things, activating nerve cells, including something called glutamate. This leakage causes nerve cells to become hyper-sensitive to stimulation or overactive, and can set off a chain reaction that further damages nerve cells. At the same time as nerve cells become hyper-sensitive to stimulation, the brain's immune cells, including microglia, which are necessary for "controlled" inflammation after trauma to the brain, are activated. This immune response is necessary to initiate the natural healing process after injury.
These dysfunctions at the cellular level in combination with the physical tensile damage to nerve fibers cause a domino effect of dysfunctions in the brain that make it more challenging to function normally.
See how the brain moves inside the skull during a direct blow to the head: https://i.imgur.com/aKiPvPl.gif
See what happens to the brain in a car accident: http://www.brainline.org/content/multimedia.php?id=848
These primary functional disorders resulting from the concussion initiate a domino effect of secondary functional disorders in both external (cortical) and internal (subcortical) parts of the brain. Including parts of the brain involved in processing and coordinating multiple sensory impressions simultaneously (multisensory integration), which are responsible for synchronizing the activation of several different centers with different properties in the brain simultaneously to perform both physical and cognitive tasks (cross modal activation), while both cortical and subcortical areas that are not normally activated during certain tasks are activated in people who have suffered a concussion and mild traumatic brain injury. Research has shown that disrupted synchronization between the brain's reception of sensory information and production of motor signals results in impaired neuroplasticity and learning. This is one of the reasons why it is very difficult to find effective treatments that can reduce symptoms and improve quality of life in children and adults with chronic concussion syndrome, post-concussion syndrome.
Neuroplasticity is the brain's ability to change and adapt throughout life by forming new connections and strengthening existing networks. This process can occur in response to learning, experience and injury and enables the brain to adapt and repair. Neuroplasticity underpins our cognitive and motor development, memory and ability to learn new skills.
fMRI and EEG show functional disturbance in the outer and inner parts of the brain in chronic concussion syndrome.

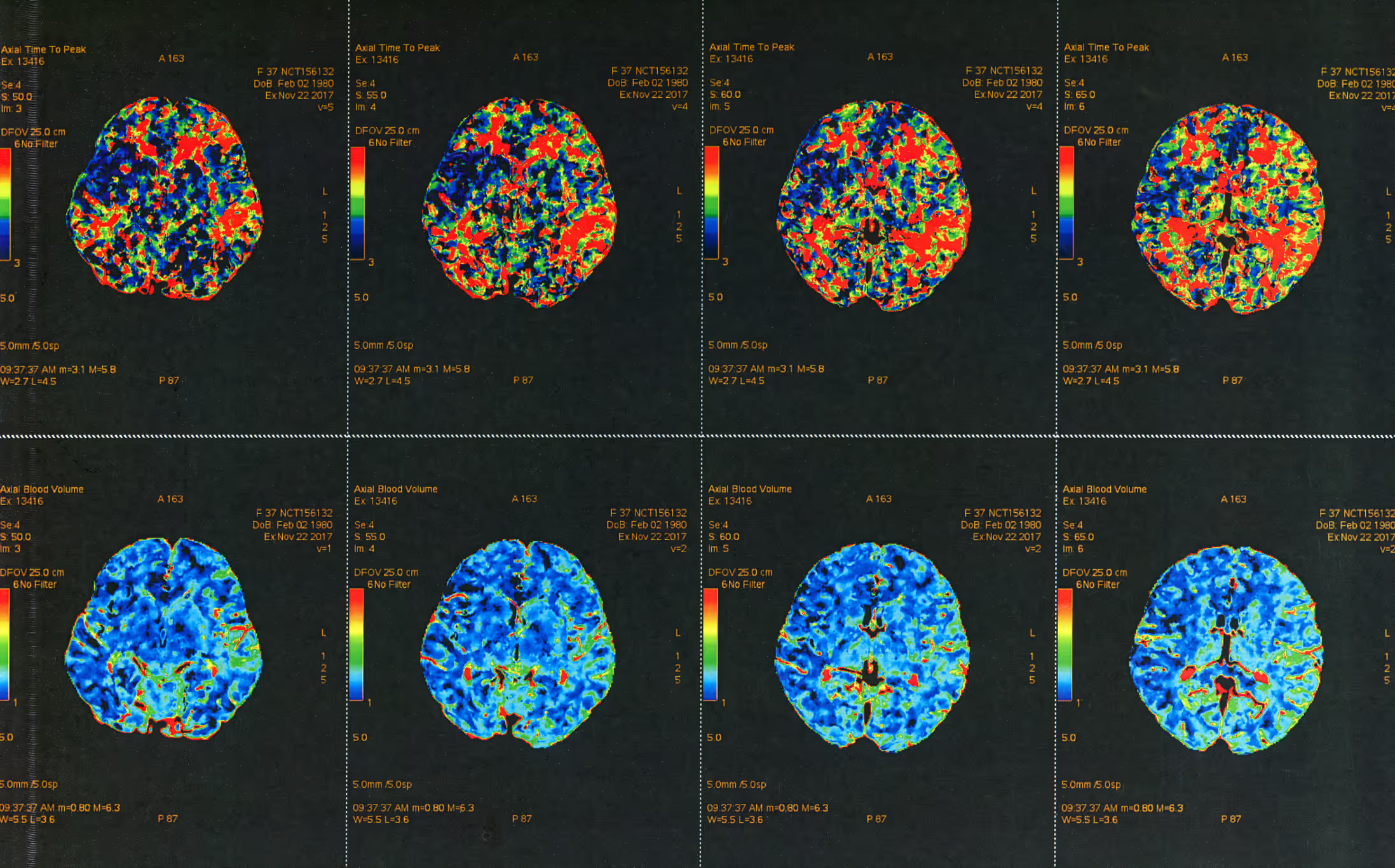

Functional magnetic resonance imaging (fMRI) shows changes in the outer (cortical) and inner (subcortical) areas of the brain in chronic concussion syndrome, post-concussion syndrome (PCS). Including reduced resting state or resting activity in the brain and changes in brain activation patterns. A study from 2020 has shown a significant reduction in functional connections between several external and internal areas. Including areas called the prefrontal cortex, superior parietal cortex and temporal cortex. These are areas that are important for, among other things, the coordination and processing of different sensory impressions, and coordination between them is important for good cognitive function and good ability to orient and move. Another study from 2019 used structural MRI (conventional MRI) to detect changes in the thickness of the outer parts of the brain in these areas in people with post-commotio syndrome.
Research using electroencephalography (EEG) has also shown functional changes in post-commotio syndrome. In 2019, changes were detected in both cortical and subcortical areas, with both increases and decreases in activity in different areas of the brain. These changes appear to be associated with impaired cognitive function in people with post-commotio syndrome. In addition, a previous study from 2018 shows that people with post-commotio syndrome have disturbances in cortical network dynamics, with a decrease in small world brain networks and increased modular organization.
Good changes to the brain's small world brain network involve adjustments to how neurons and their connections are organized so that information can be transferred efficiently and effortlessly. These changes can lead to increased information flow and improved cognitive function, and can be the result of learning, experience or healing processes after injury. Good regulation of this network contributes to neuroplasticity and the brain's ability to adapt to different situations and demands. Disruptive changes resulting from an injury, disease or developmental disorder reduce the brain's capacity for neuroplasticity, making it more challenging and energy demanding to adapt to new situations.
Modular organization in the brain refers to the way neurons and their connections are grouped into separate but functionally related clusters, called modules. These modules are specialized to process different types of information or perform specific tasks. Modular organization contributes to efficient information processing, as modules can work independently while interacting with other modules when necessary. This network of modules enables rapid and flexible adaptation to new situations and learning experiences, contributing to neuroplasticity and the brain's ability to adapt and evolve. In people with post-commotio syndrome, there is increased modular organization, probably as a result of a number of compensatory mechanisms in an attempt to compensate for primary and secondary functional impairments.
Function and dysfunction in the outer and inner parts of the brain.
To gain a better understanding of what happens in the brain in a concussion and what causes the wide range of symptoms associated with a concussion, we need to review the functions of some of the areas of the brain and what happens to them in a head trauma. We will do this in part 2 of this article which will be published in a few weeks.

Reference list:
1. badre, D., & Frank, M. J. (2020). Interactions between prefrontal cortex and basal ganglia during decision making. Nature Reviews Neuroscience, 21(12), 691-705.
2 Bertolini, G., & Tarnutzer, A. A. (2020). The neural basis of spatial orientation and its modulation by multisensory and vestibular input. Journal of Neurophysiology, 124(3), 738-751.
3. betzel, R. F., Medaglia, J. D., & Bassett, D. S. (2020). Diversity of meso-scale architecture in human and non-human connectomes. Nature Communications, 11(1), 1-13. This study explores the organization of "small world" networks in human
4 Buki A, Egyud L, Okonkwo DO, et al. Update on mild traumatic brain injury: an introduction to diagnosis and management. J Neurol Neurosurg Psychiatry. 2021;92(2):219-227. doi:10.1136/jnnp-2020-323628
5 Cai, Y., et al. "Decreased functional connectivity density in subjects with post-concussion syndrome." Frontiers in neurology 9 (2018): 572.
6 Chen, J. K., et al. "A prospective study of white matter abnormalities in mild traumatic brain injury at the acute stage." Neurology 89.15 (2017): 1562-1571.
7 Davenport, N. D., et al. "Abnormalities in visual and auditory cortical activation in mild traumatic brain injury." Journal of the International Neuropsychological Society 25.1 (2019): 26-37.
8 De Beaumont L, Tremblay S, Lassonde M, Théoret H. Long-term and cumulative effects of sports concussion on motor cortex inhibition. Neurosurgery. 2021;89(Suppl_1):S34-S42. doi:10.1093/neuros/nyaa527
9 Delaney, J. S., et al. "Balance and vestibular dysfunction in individuals with persistent post-concussion syndrome." Journal of head trauma rehabilitation 34.4 (2019): E28-E36.
10 Faghri PD, Rodrigues E, Lo CK, Yost RA. Virtual reality-based cognitive-motor rehabilitation in persons with traumatic brain injury: a pilot study. Am J Phys Med Rehabil. 2020;99(6):515-522. doi:10.1097/PHM.0000000000001398
11. Figueiredo, T. H., et al. "Altered resting-state connectivity in post-concussion syndrome: a pilot study." Brain Injury 33.1 (2019): 114-121.
12 Frederick R. Carrick et al, 2012. Whole body rotation omitting a multi-axial rotational chair in case of multiple system atrophy-like syndrome. Functional Neurology, Rehabilitaiton and Ergonomics. Vol 2, No 1, 2012.
13. Frederick R. Carrick wt al, 2011, The effect of whole body rotations in the pitch and yaw planes on postural stability. Functional Neurology, Rehabilitaiton and Ergonomics. Vol 2, 167-179, 2011.
14 Frederick R. Carrick et al, 2015. Evaluation of the effectiveness of novel brain and vestibular rehabilitation treatment modality in PSTD patients who have suffered combat-related traumatic brain injuries. Frontiers in Public Health vol 3 (2015), article 15.
15 Frederick R. Carrick et al, 2015. Short- and long-term effectiveness of a subject's specific novel brain and vestibular rehabilitation treatment modality in combat veterans suffering PTSD. Frontiers in Public Health vol 3 (2015), article 151.
16. furlan, L., & Krüger, O. (2020). Involvement of the human ventromedial prefrontal cortex in goal-directed motor planning. eLife, 9, e57737.
17 Giza CC, Hovda DA. The new neurometabolic cascade of concussion. Neurosurgery. 2021;89(Suppl_1):S24-S33. doi:10.1093/neuros/nyaa523
18 Guo, Z., Li, A., & Yu, L. (2020). Neural mechanisms underlying the integration of situational information into attribution outcomes. Human Brain Mapping, 41(6), 1506-1518.
19. Directorate of Health
20. hilgetag, C. C., & Goulas, A. (2020). Is the brain really a small-world network?. Brain Structure and Function, 225(2), 647-660.
21 Hoffman, N. L., et al. "Vestibular dysfunction in post-concussive syndrome." Journal of neurologic physical therapy: JNPT 43.4 (2019): 214-221.
22 Huang C, Duan K, Hu S, et al. Dysregulation of the immune system in post-concussion syndrome. Front Neurol. 2021;12:676727. doi:10.3389/fneur.2021.676727
23 Jeannie Ponsford et al, 1999. Cognitive and Behavioral Outcome Following Mild Traumatic Head Injury in Children. Journal of Head Trauma Rehabilitation, August 1999.
24 Kheradmand, A., & Winnick, A. (2020). Vestibular control of standing balance is enhanced with increased cognitive load. Frontiers in Neurology, 11, 566.
25 Kim, Y. W., et al. "Altered cortical thickness in patients with post-concussion syndrome: a structural magnetic resonance imaging study." Journal of Neurotrauma 36.2 (2019): 306-312.
26. kim, H. E., Morehead, J. R., Parvin, D. E., Moazzezi, R., & Ivry, R. B. (2020). Inhibition of saccades elicits attentional suppression and retinotopic adaptation in human visual cortex. Journal of Neuroscience, 40(14), 2889-2901.
27 King, L. A., et al. "Persistent symptoms and activity changes three months after mild traumatic brain injury." Journal of rehabilitation research and development 55.3 (2018): 305-314.
28. kromrey, S., Haarmeier, T., & Thier, P. (2020). Neural basis of the saccadic suppression of displacement detection. Cerebral Cortex, 30(6), 3586-3598.
29 Kumar, A., et al. "Alterations in functional connectivity of small-world brain networks in patients with mild traumatic brain injury." PloS one 13.10 (2018): e0205549.
30 Leddy, J.J., Haider, M.N., Ellis, M.J., et al. (2021). "Early Subthreshold Aerobic Exercise for Sport-Related Concussion: A Randomized Clinical Trial." Journal of Neurotrauma, 38(4), 479-487.
31 Leddy, J.J., Haider, M.N., Hinds, A., et al. (2022). "Early Exercise After Sport-Related Concussion: A Systematic Review and Meta-Analysis." British Journal of Sports Medicine, 56(4), 192-197.
32 Leddy, J. J., et al. "A preliminary study of the effect of early aerobic exercise treatment for sport-related concussion in males." Clinical Journal of Sport Medicine 28.1 (2018): 13-21.
33 Mannix R, Meehan WP, Monuteaux MC, et al. Clinical predictors of prolonged recovery after concussion in children and adolescents. JAMA Pediatrics. 2020;174(2):e195905. doi:10.1001/jamapediatrics.2019.5905
34 Mark E. Halstead et al, 2010. Sport-Related Concussion in Children and Adolescents. Pediatrics volume 126, number 3, September 2010.
35 Matthew T. Neal et al, 2011. Concussions: What a neurosurgeon should know about current scientific evidence and management strategies. Surgical Neurology International 2012; 3:16.
36 Maugans TA, Farley C, Altaye M, Leach J, Cecil KM. Pediatric sports-related concussion produces cerebral blood flow alterations. Pediatrics. 2020;146(2):e20193980. doi:10.1542/peds.2019-3980
37 McCrea, M., Meier, T., Huber, D., et al. (2020). "Role of Advanced Imaging in Sport-Related Concussion." Journal of Head Trauma Rehabilitation, 35(1), 1-8.
38 McDougle, S. D., & Taylor, J. A. (2020). Dissociable cognitive strategies for sensorimotor learning. Nature Communications, 11(1), 1-13.
39 Meier TB, Karr JE, Karr JW, et al. Mild traumatic brain injury in the United States military: epidemiology, risk factors, and mitigation strategies. Curr Opin Neurol. 2021;34(6):709-714.
40. niv, Y., & Langdon, A. (2021). Reinforcement learning with continuous actions through model-based planning. Journal of Neuroscience, 41(1), 5-15.
41 Norwegian Health Information, Norwegian patient handbook.
42 Patel R, Sampaio-Baptista C, Johansen-Berg H. Structural and functional plasticity following concussion. Neurosci Lett. 2020;725:134902. doi:10.1016/j.neulet.2020.134902
43 Perrault, T. J., et al. "Superior colliculus neuronal responses to multisensory stimuli in post-concussive syndrome." Journal of Neurotrauma 36.5 (2019): 791-802.
44. salari, E., Bütefisch, C. M., & Zimerman, M. (2020). Investigating the neural basis of theta burst stimulation to premotor cortex on emotional facial expression recognition: role of the mirror neuron system. Scientific Reports, 10(1), 1-10.
45 Schneider, K.J., Meeuwisse, W.H., Nettel-Aguirre, A., et al. (2023). "Rest and Return to Activity After Sport-Related Concussion: A Systematic Review and Meta-analysis." British Journal of Sports Medicine, 57(1), 3-8.
46 Seabury, S. A., et al. "Neuroimaging correlates and predictors of symptom improvement following concussion in a pediatric population." Journal of Neurotrauma 36.22 (2019): 3182-3192.
47 Schneiderman, A. I., et al. "Relationship between history of traumatic brain injury and recent risky driving behavior: a population-based study." The Journal of the American Medical Association 296.9 (2006): 2574-2581.
48 Shahim, P., et al. "Multimodal assessment of neurodegeneration in post-concussion syndrome after mild traumatic brain injury: a prospective longitudinal study." Journal of Neurology, Neurosurgery & Psychiatry 91.3 (2020): 265-276.
49 Shumskaya E, Andriessen TMJC, Norris DG, Vos PE. Abnormal neuronal activation after concussion in the absence of structural abnormalities on conventional neuroimaging. J Neurol Neurosurg Psychiatry. 2021;92(2):170-177. doi:10.1136/jnnp-2020-323558.
50 Shumskaya, E., et al. "Diffuse white matter abnormalities in chronic mild traumatic brain injury and their relationship to neuropsychological functioning." NeuroImage: Clinical 21 (2019): 101632.
51 Smith, P. F., & Zheng, Y. (2020). From ear to uncertainty: vestibular contributions to cognitive function. Frontiers in Integrative Neuroscience, 14, 4.
52 Snellman M, Ramberg E, Lindqvist J, et al. Genetic variation associated with concussion susceptibility in Swedish ice hockey players. PLoS One. 2021;16(2):e0247558. doi:10.1371/journal.pone.0247558
53 Timothy Belton and Robert A. McCrea (2000). Role of the Cerebellar Flocculus Region in Cancellation of the VOR During Passive Whole body Rotation. Journal of Neurophysiology, 84: 1599-1613, 2000.
54 Tremblay, S., & Small, S. L. (2020). Motor learning and the covert practice of movement. Journal of Neuroscience, 40(50), 9552-9560.
55. van der Horn, H. J., et al. "Structural connectivity changes in post-concussion syndrome: a diffusion tensor imaging study." NeuroImage: Clinical 22 (2019): 101707.
56 Wu, Y., et al. "Cerebellar gray matter reductions associate with decreased functional connectivity in the vestibular cerebellum in patients with persistent postural-perceptual dizziness." Journal of Neurology 266.8 (2019): 1993-2003.
57 Y.P. Ivanenko et al, 1997. The contribution of otoliths and semicicular canals to the perception of two-dimensional passive whole-body motion in humans. Journal of physiology, 502. 1, pp. 223-233, 1997.
58 Yuh EL, Mukherjee P, Lingsma HF, et al. Magnetic resonance imaging improves 3-month outcome prediction in mild traumatic brain injury. Ann Neurol. 2021;89(1):49-59. doi:10.1002/ana.25920
59 Yuan, W., et al. "Functional connectivity changes in mild traumatic brain injury assessed using resting-state functional magnetic resonance imaging." The Journal of Neuropsychiatry and Clinical Neurosciences 31.1 (2019): 47-53.
60 Zatorre, R. J., & Fields, R. D. (2020). Neuroscience: Can musical training change the brain?. Current Biology, 30(13), R722-R724.
61 Zhou, Y., et al. "EEG source imaging correlates of mild traumatic brain injury recovery trajectories." Brain 142.3 (2019): 633-646.
62. zhu, D. C., et al. "Altered resting state connectivity in persistent post-concussive symptoms following mild traumatic brain injury: a network analysis." NeuroImage: Clinical 20 (2018): 18-27.
63 Zu Eulenburg, P., & zu Eulenburg, C. (2020). Cortical networks of the human vestibular cortex: Evidence from structural and functional connectivity studies. Brain Structure and Function, 225(3), 801-814.