Concussion in children

Bumps and falls are part of being a child, playing games and sports, and fortunately most of them are fine. However, in some cases, the fall is so hard that the child suffers a concussion and long-term problems.
As mentioned in our first post on concussion, concussion is the most common head injury following physical trauma and affects over 30 000 Norwegians every year. Concussion occurs when physical trauma causes an impact injury to the brain. Either by direct blows or impacts to the head or neck, or by other forms of physical trauma that cause indirect impacts to the brain such as landing heavily on the buttocks. In children, this usually happens during play or sports activities, but unfortunately also after violent incidents or accidents. This blow, or impact to the brain, can lead to an immediate disruption of brain function. In the majority of cases, this is transient within 1-3 months, but over 40% of concussion cases suffer long-term effects for over 5 years.
As a child's brain is still developing, the consequences of a concussion can be different from those of adults. A child's brain has different developmental milestones that can be affected by physical and psychological trauma. This can mean that children can have very good and rapid recovery, or that trauma can cause maturational abnormalities in the brain that become more apparent at later ages. It is suspected that these maturational disturbances may become more prominent as social, academic and physical challenges become more demanding with age. This means that the age at which the child is exposed to head trauma may affect the extent to which the concussion can cause late effects. The child may show mild symptoms and seem to function well in school or extracurricular activities for the first few weeks or months. But as it becomes more demanding, the child may start to lag behind average development.
A study back in 1999 observed 130 children and adolescents between 6 and 15 years of age, 1 week and 3 months after they sustained a concussion. Of the 130 cases, 17% suffered significant long-term symptoms for more than 3 months. Another study from 2021 shows that concussions in children can have a negative impact on cognitive development and lead to learning difficulties, among other things. A 2022 study shows that children can have structural changes in their brains that last up to 4 months after a concussion. Fortunately, most children and young people who suffer a concussion do well. In the vast majority of cases, symptoms and discomfort will be gone within a week, up to 1-3 months. However, in as many as over 25% of children and young people who sustain a concussion suffer long-term symptoms that last more than 6 months and reduce their quality of life and development.
Symptoms of concussion
When a child is subjected to physical trauma that causes direct or indirect impact to the brain and that causes the development of neurological symptoms immediately after the injury, or minutes or hours after, can be defined as a concussion. Including physical symptoms, cognitive disturbances, and behavioral changes.
- Headache
- Dizziness
- Brain fog
- Nausea
- High sensitivity to sensory input
- Stiffness and pain in the back and neck
- Impaired balance and coordination
- Ear infection
- Fatigue
- Irritability and mood swings
- Confusion
- Impaired attention and responsiveness
- Impaired concentration
- Memory impairment
- Sleep disorder
- Reduced threshold to sensory input and activity before symptoms worsen
What do you do when you suspect a concussion?
Safety is very important for children who have suffered physical trauma that can cause concussions.
- It is important that one person stays with the child while others call for help.
- If the child has not regained consciousness or is still confused (disoriented), place the child in a stable lateral position to ensure a free airway and call 113 immediately.
- It is important to talk to the child calmly and make sure the child is breathing calmly and conscious.
- If the child is sleepy and wants to sleep, the child should be woken up every 15 minutes for mild concussion to check that it is just natural sleep and not loss of consciousness.
- It is also important not to give the child fluids immediately after head trauma as this can increase the risk of vomiting.
- In all cases where the child has lost consciousness, even for a few minutes, or is confused (disoriented), emergency services should be contacted to rule out serious injury.
- If there is any doubt as to whether the injury is serious, contact the emergency services.
- Concussion itself is not dangerous, but in cases of head trauma it is important to rule out conditions such as swelling of the brain or cerebral hemorrhage.
Treatment of acute concussion
The immediate treatment for children with concussion is rest and monitoring for the first 24-48 hours. The first night it is important to wake the child once every 2-3 hours and ask questions such as name, date of birth and where they live to test for consciousness. It is also important to avoid moderate-hard physical activity, reading, watching TV/PC/tablet etc. and one must stay away from mental work that exacerbates symptoms for the first 2-7 days. All these activities can exhaust the brain and one risks prolonging the course of symptoms if one returns too soon to "normal" activity and does not pay attention to the symptoms. It is also important to avoid painkillers for the first 48 hours even if there is a lot of discomfort or pain. All medication for children must be supervised by a doctor. This is important because painkillers can mask worsening symptoms caused by swelling in the brain and can affect the blood's ability to clot. If the child complains a lot of discomfort or any of the symptoms worsen, contact an emergency room.
Rest is important in the first week after a concussion, but inactivity and isolation from exposure to common sensory stimuli encountered in everyday life can exacerbate the condition and prolong the course of symptoms. It is therefore important to gradually increase activity and exposure to sensory input, but take into account tolerance before symptoms are triggered or exacerbated.
If the child is not symptom-free and back to normal activity within 3 months, the child falls into the category of chronic concussion syndrome, post-concussion syndrome. Children with chronic concussion syndrome may be bothered by symptoms for several years and, as mentioned earlier, this can affect the child's development.
It is common to see a decline in grades in children and young people with late effects of concussion. Evidence suggests that children and young people who suffer repeated concussions increase their risk of long-term problems.

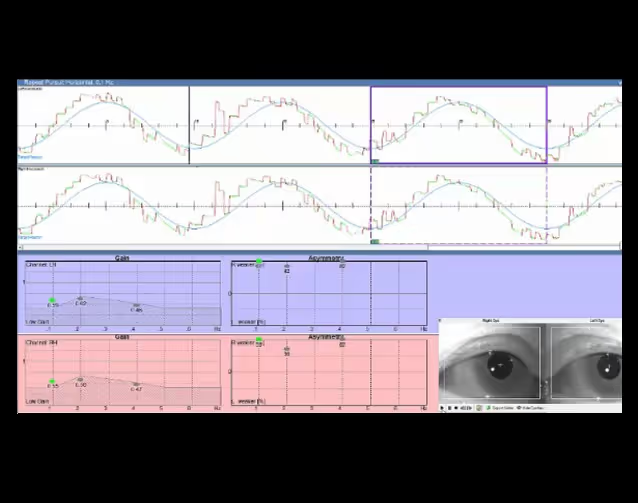
Brain Camp and Kim Tore Johansen have long and broad experience in examining and adapting neurological rehabilitation that can improve symptoms resulting from chronic concussion syndrome and other acquired brain injuries in children and adolescents. Among other things, we use computer-based tests that measure fine motor control over purposeful eye movements.
Reference list:
- Andrew R. Mayer et al, 2023. Prospective study of grey matter atrophy followingpediatric mild traumatic brain injury. Neurology, 100 (5), 2023. DOI:
https://doi.org/10.1212/WNL.0000000000201470
- Baugh, C.M., & Fratelli, M. (2020). Sports-related concussion in children and adolescents.Pediatric Clinics of North America, 67(3), 735-749.
- Caeyenberghs,K., Leemans, A., Durand, J. B., Leclercq, Y., & Swinnen, S. P. (2020). Theimpact of traumatic brain injury on neural networks in children andadolescents: A review.
Neuropsychology Review, 30(3), 230-247.
- Coats, B.S., & Dietrich, A. (2004). The long-term impact of pediatric head injury onacademic achievement, behavior, and emotional functioning. Journalof School Psychology, 42(3), 213-
232.
- DeBellis, M. D., Keshavan, M. S., & Shifflett, H. (2020). Traumatic braininjury in children and adolescents: An overview of the impact on braindevelopment. Journal of Neuropsychiatry and
Clinical Neurosciences, 32(2),E1-E10.
- E.Helseth and K. K. Anda. Treatment of concussion (commotio cerebri) in children. Oslo University Hospital.
- Directorate of Health
- Jeannie Ponsford et al, 1999. Cognitive and BehavioralOutcome Following Mild Traumatic Head Injury in Children. Journal of Head Trauma Rehabilitation, August 1999.
- Johnson,R. (2009). Late outcomes after pediatric head injury. DevelopmentalDisabilities Research Reviews, 15(3), 209-216.
- Mark E.Halstead et al, 2010. Sport-Related Concussion in Children and Adolescents. Pediatrics volume 126, number 3, september2010.
- Matthew T. Neal et al, 2011. Concussions: What aneurosurgeon should know about current scientific evidence and managementstrategies. SurgicalNeurology International 2012; 3:16.
- Norwegian Health Information, Norwegian patient handbook.
- Ponsford,J. (2020). Cognitive and emotional outcomes after traumatic brain injury inchildren and adolescents. Child and Adolescent Psychiatric Clinics ofNorth America, 29(4), 577-
588.
- Slick, D. J., Matson, S. J., & Maerlender, A. C. (2020). Pediatric traumatic brain injury: Assessment,management, and outcomes. Child and Adolescent Psychiatric Clinics of North
America, 29(4), 553-576.
- Taylor,H. G., & Dodge, N. A. (2010). Traumatic brain injury in children andadolescents. Current Opinion in Pediatrics, 22(4), 394-401.
- Teng, E. L., & Chugani, D. C. (1998). Pediatric traumatic brain injury: A criticalreview of the past 10 years. Journal of Head Trauma Rehabilitation, 13(4),61-73.
- Vicki Anderson et al, 2011. Do Children really recoverbetter? Neurobehavioral plasticity after early brain insult. Brain 2011: 134; 2197-2221.
- Yeates,K. O., & Ris, M. D. (2010). Long-term outcomes of traumatic brain injury in children and adolescents. Current Opinion in Pediatrics, 22(4),402-408.